|
|
|
|
|
|
|
USO
DI STATINE E INCIDENZA DI ALZHEIMER
[STATINS, INCIDENT ALZHEIMER DISEASE, CHANGE IN COGNITIVE
FUNCTION, AND NEUROPATHOLOGY. Neurology, pubblicato on line il 16
gennaio 2008]
ABSTRACT
OBJECTIVE To examine the relation of statins to incident
Alzheimer disease (AD) and change in cognition and neuropathology.
METHODS Participants were 929 older Catholic clergy (68.7%
women, mean baseline age 74.9 years, education 18.2 years, Mini-Mental
State Examination 28.5) free of dementia, enrolled in the Religious
Orders Study, a longitudinal clinical-pathologic study of AD. All
agreed to brain autopsy at time of death and underwent annual structured
clinical evaluations, allowing for classification of AD and assessment
of cognition (based on 19 neuropsychological tests). Statins were
identified by direct medication inspection. Neuropathologic data
were available on 262 participants. All macroscopic chronic cerebral
infarctions were recorded. A measure of global AD pathology was
derived from silver stain, and separate measures of amyloid and
tangles were based on immunohistochemistry. We examined the relation
of statins to incident AD using Cox proportional hazards, change
in cognition using mixed effects models, and pathologic indices
using logistic and linear regression.
RESULTS Statin use at baseline (12.8%) was not associated
with incident AD (191 persons, up to 12 follow-up years), change
in global cognition, or five separate cognitive domains (all p values
> 0.20). Statin use any time prior to death (17.9%) was not related
to global AD pathology. Persons taking statins were less likely
to have amyloid (p = 0.02). However, among those with amyloid, there
was no relation of statins to amyloid load. Statins were not related
to tangles or infarction.
CONCLUSIONS Overall, statins were not related to incident
Alzheimer disease (AD) or change in cognition, or continuous measures
of AD pathology or infarction.
|
|
|
|
|
|
TRATTAMENTO
CON EPARINA E RISCHIO DI EVENTI CV
[INCIDENCE AND PROGNOSTIC SIGNIFICANCE OF THROMBOCYTOPENIA
IN PATIENTS TREATED WITH PROLONGED HEPARIN THERAPY. Arch Intern
Med 2008; 168:94-102]
ABSTRACT
BACKGROUND Despite widespread heparin use in clinical practice,
the associated development of thrombocytopenia is an underrecognized
and undertreated complication.
METHODS We analyzed data from consecutive hospitalized
patients treated with heparin (unfractionated or low molecular
weight) for 4 days or longer to determine the incidence, predictors,
prognostic significance, and management of "thrombocytopenia,"
defined as a platelet count less than 150 x 10(9)/L, reduction
in platelet count of 50% or more from the admission level, or
both.
RESULTS We enrolled 2420 patients (median age, 65.2 years;
43.8% women) in 48 US hospitals. Thrombocytopenia occurred in
881 patients (36.4%; 95% confidence interval [CI], 34.5%-38.3%).
Of those who developed thrombocytopenia, 5.1% died, compared with
1.6% of those without thrombocytopenia (odds ratio [OR], 3.4;
95% CI, 2.1-5.6; P < .001). Thrombocytopenia was also associated
with greater risk of myocardial infarction (OR, 2.1; 95% CI, 1.5-2.8;
P < .001) and congestive heart failure (OR, 1.3; 95% CI, 1.1-1.6;
P = .01). After adjustment for important covariates, thrombocytopenia
remained an independent predictor of thrombotic and hemorrhagic
events. A relative reduction in platelet count of more than 70%
was the strongest independent predictor of death (OR, 13.4; 95%
CI, 6.5-27.6; P < .001), followed by a relative reduction in
platelet count of 50% to 70%, worse Killip class, occurrence of
thromboembolic complications, older age, and longer duration of
heparin therapy.
CONCLUSIONS Thrombocytopenia occurs frequently after prolonged
heparin therapy and is strongly associated with worse short-term
clinical outcome. The relative reduction in platelet count is
a powerful independent predictor of all-cause mortality in hospitalized
patients.
In-hospital
outcomes insofar as development of thrombocytopenia.
MI myocardial infarction; CHF, congestive heart failure
|
|
|
|
|
|
CONTRACCETTIVI
ORALI E CANCRO OVARICO
[OVARIAN CANCER AND ORAL CONTRACEPTIVES: COLLABORATIVE
REANALYSIS OF DATA FROM 45 EPIDEMIOLOGICAL STUDIES INCLUDING 23,257
WOMEN WITH OVARIAN CANCER AND 87,303 CONTROLS. The Lancet 2008;
371:303-314]
SUMMARY
BACKGROUND Oral contraceptives were introduced almost 50
years ago, and over 100 million women currently use them. Oral contraceptives
can reduce the risk of ovarian cancer, but the eventual public-health
effects of this reduction will depend on how long the protection
lasts after use ceases. We aimed to assess these effects.
METHODS Individual data for 23,257 women with ovarian cancer
(cases) and 87,303 without ovarian cancer (controls) from 45 epidemiological
studies in 21 countries were checked and analysed centrally. The
relative risk of ovarian cancer in relation to oral contraceptive
use was estimated, stratifying by study, age, parity, and hysterectomy.
FINDINGS Overall 7308 (31%) cases and 32,717 (37%) controls
had ever used oral contraceptives, for average durations among users
of 4.4 and 5.,0 years, respectively. The median year of cancer diagnosis
was 1993, when cases were aged an average of 56 years. The longer
that women had used oral contraceptives, the greater the reduction
in ovarian cancer risk (p<0·0001). This reduction in risk
persisted for more than 30 years after oral contraceptive use had
ceased but became somewhat attenuated over time-the proportional
risk reductions per 5 years of use were 29% (95% CI 23-34%) for
use that had ceased less than 10 years previously, 19% (14-24%)
for use that had ceased 10-19 years previously, and 15% (9-21%)
for use that had ceased 20-29 years previously. Use during the 1960s,
1970s, and 1980s was associated with similar proportional risk reductions,
although typical oestrogen doses in the 1960s were more than double
those in the 1980s. The incidence of mucinous tumours (12% of the
total) seemed little affected by oral contraceptives, but otherwise
the proportional risk reduction did not vary much between different
histological types. In high-income countries, 10 years use of oral
contraceptives was estimated to reduce ovarian cancer incidence
before age 75 from 1.2 to 0.8 per 100 users and mortality from 0.7
to 0.·5 per 100; for every 5000 woman-years of use, about
two ovarian cancers and one death from the disease before age 75
are prevented.
INTERPRETATION Use of oral contraceptives confers long-term
protection against ovarian cancer. These findings suggest that oral
contraceptives have already prevented some 200,000 ovarian cancers
and 100,000 deaths from the disease, and that over the next few
decades the number of cancers prevented will rise to at least 30,000
per year.
|
|
|
|
|
|
RISCHIO DI IPERTENSIONE: UN NUOVO RISK
SCORE DALLO STUDIO FRAMINGHAM
[A RISK SCORE FOR PREDICTING NEAR-TERM INCIDENCE
OF HYPERTENSION: THE FRAMINGHAM HEART STUDY. Ann Intern Med. 2008;
148:102-10]
ABSTRACT
BACKGROUND Studies suggest that targeting high-risk, nonhypertensive
individuals for treatment may delay hypertension onset, thereby
possibly mitigating vascular complications. Risk stratification
may facilitate cost-effective approaches to management.
OBJECTIVE To develop a simple risk score for predicting
hypertension incidence by using measures readily obtained in the
physician's office.
DESIGN Longitudinal cohort study.
SETTING Framingham Heart Study, Framingham, Massachusetts.
PATIENTS 1717 nonhypertensive white individuals 20 to 69
years of age (mean age, 42 years; 54% women), without diabetes
and with both parents in the original cohort of the Framingham
Heart Study, contributed 5814 person-examinations.
MEASUREMENTS Scores were developed for predicting the 1-,
2-, and 4-year risk for new-onset hypertension, and performance
characteristics of the prediction algorithm were assessed by using
calibration and discrimination measures. Parental hypertension
was ascertained from examinations of the original cohort of the
Framingham Heart Study.
RESULTS During follow-up (median time over all person-examinations,
3.8 years), 796 persons (52% women) developed new-onset hypertension.
In multivariable analyses, age, sex, systolic and diastolic blood
pressure, body mass index, parental hypertension, and cigarette
smoking were significant predictors of hypertension. According
to the risk score based on these factors, the 4-year risk for
incident hypertension was classified as low (<5%) in 34% of
participants, medium (5% to 10%) in 19%, and high (>10%) in
47%. The c-statistic for the prediction model was 0.788, and calibration
was very good.
LIMITATIONS The risk score findings may not be generalizable
to persons of nonwhite race or ethnicity or to persons with diabetes.
The risk score algorithm has not been validated in an independent
cohort and is based on single measurements of risk factors and
blood pressure.
CONCLUSION The hypertension risk prediction score can be
used to estimate an individual's absolute risk for hypertension
on short-term follow-up, and it represents a simple, office-based
tool that may facilitate management of high-risk individuals with
prehypertension.
Calculation
of scores to predict 1-, 2-, and 4-year risk for new-onset hypertension.
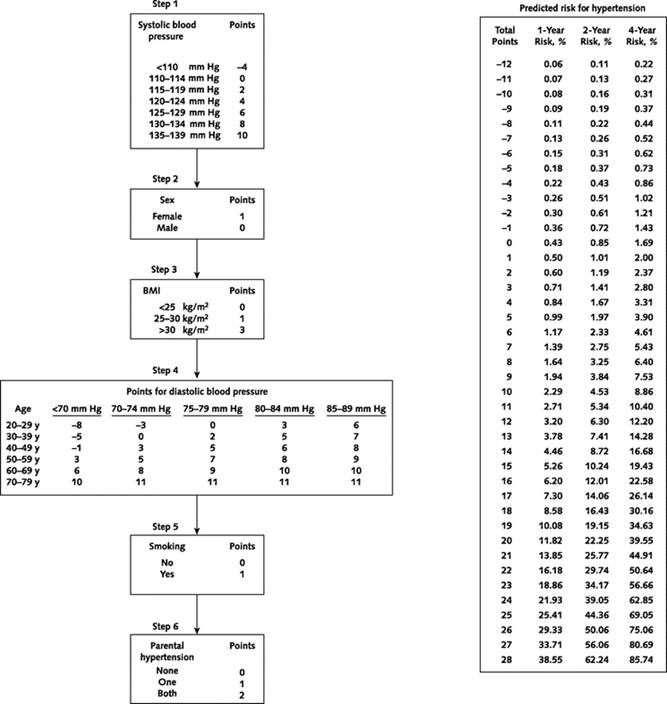
Four-year
predicted probability of hypertension in men and women, by selected
risk factors.
Blood
pressure was 120/80 mm Hg, unless otherwise indicated.
Plus and minus signs below graph indicate the presence or absence
of risk factors.
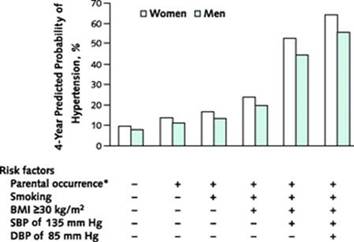
BMI
body mass index; DBP diastolic blood pressure; SBP systolic blood
pressure
*Both parents with hypertension
|
|
|
|
|
|
INDICE
DI RISCHIO PROGNOSTICO PER LA MORTALITÀ A LUNGO TERMINE
DA ARTEROPATIA PERIFERICA
[A PROGNOSTIC RISK INDEX FOR LONG-TERM MORTALITY
IN PATIENTS WITH PERIPHERAL ARTERIAL DISEASE. Arch Intern Med.
2007;167:2482-2489]
ABSTRACT
STUDY QUESTION Can an accurate and easy-to-use prognostic
risk index for long-term mortality in patients with peripheral
artery disease (PAD) be developed?
METHODS The authors reviewed data from their center, including
consecutive patients with PAD who were referred to the Department
of Vascular Medicine at the Erasmus Medical Center between January
1983 and August 2005. Subjects with ankle-brachial index (ABI)
>0.90 were excluded. This cohort was then divided into derivation
and validation sets. Regression analysis with stepwise backwards
elimination was used to identify predictors of 1-, 5-, and 10-year
mortality in the derivation cohort. Weighted points were assigned
to significant predictors. A risk index was then determined in
both the derivation and validation cohorts.
RESULTS A total of 2,642 patients with ABI <0.90 were
divided into derivation (n = 1,332) and validation (n = 1,310)
cohorts. During 10-year follow-up, mortality was 42.2% and 40.4%
in the derivation and validation cohorts, respectively. The risk
index based on beta coefficients in the regression models identified
renal dysfunction (+12), heart failure (+7), ST-segment changes
on electrocardiogram (+5), age >65 (+5), hypercholesterolemia
(+5), and ABI <0.6 (+4), Q-waves, diabetes (+3), cerebral vascular
disease (+3), and pulmonary disease (+3) as risks factors. Statin
use, aspirin, and beta-blockers were associated with a reduction
in 10-year mortality, and given negative points in the risk score.
Patients were then stratified into low, intermediate, and high
risk based on the number of points (<0, 0-5, and 6-9 points,
respectively) as well as a high-risk category for those subjects
with >9 points. The 10-year mortality rates were 22.1%, 32.2%,
45.8%, and 70.4% in these four risk groups, respectively (p <
0.001). There were comparable mortality rates in the derivation
and validation cohorts. C statistics were 0.72 and 0.73 for the
derivation and validation cohorts, respectively.
CONCLUSIONS The authors concluded that a prognostic risk
index for long-term mortality effectively stratified patients
with PAD into risk categories. They imply that this may be a useful
tool for risk stratification, counseling, and medical decision
making.
PERSPECTIVE This study is important for a couple of reasons.
First, this is a large cohort of PAD patients who were followed
for long periods of time, lending legitimacy to the long-term
predictability of this risk score. Second, this study provides
not only a useful clinical tool, but validates the importance
and relative weight of different risk factors for mortality in
patients with PAD. (It is very important to note that renal dysfunction
is the most potent predictor of mortality in patients with PAD.)
This index would allow clinicians to identify subjects who might
benefit from extremely aggressive risk factor intervention.
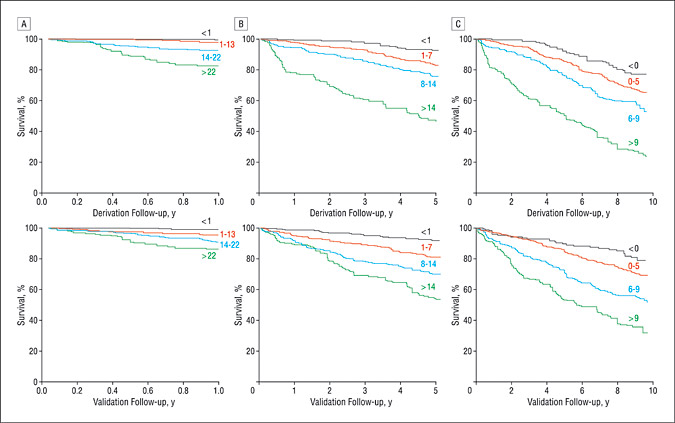
Mortality
rates at 1-year (A), 5-year (B), and 10-year (C) follow-up in
the derivation and validation cohorts, stratified according to
4 different risk classification groups (low, low-intermediate,
high-intermediate, and high risk group).
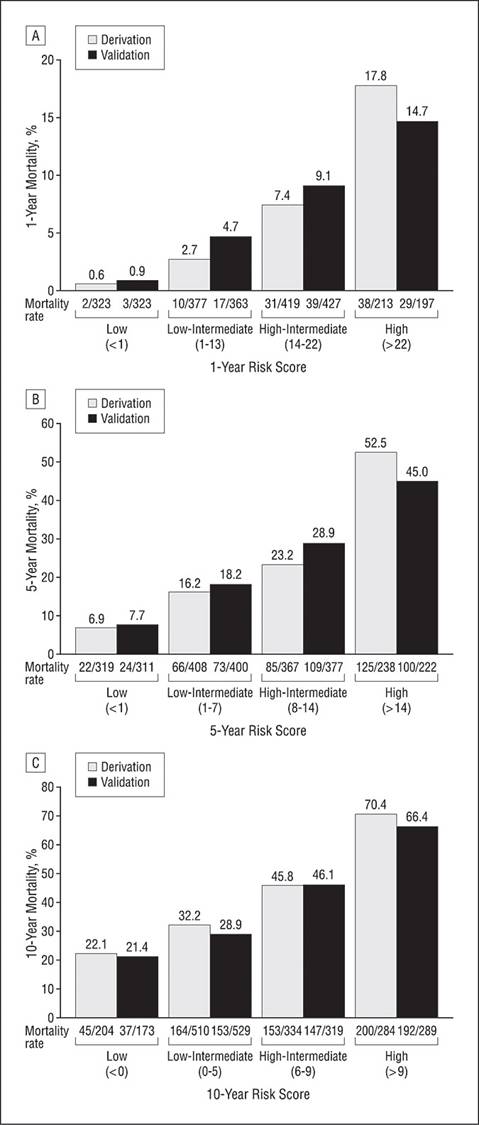
Kaplan-Meier
curves for 1-year (A), 5-year (B), and 10-year (C) survival in
the derivation and validation cohorts stratified according to
4 different risk classification groups by risk score (low, low-intermediate,
high-intermediate, and high risk).
|
|
|
|
|
|
VALORE
PREDITTIVO DELLA CALCIFICAZIONE CORONARICA PER FUTURI EVENTI CARDIACI
[PREDICTIVE VALUE OF CORONARY CALCIFICATIONS FOR FUTURE CARDIAC
EVENTS IN ASYMPTOMATIC INDIVIDUALS. Am Heart J 2008; 155:154-60]
ABSTRACT
BACKGROUND Reliable risk stratification is crucial for
efficient prevention of coronary artery disease. The following
prospective study determined the predictive value of coronary
calcifications for future cardiovascular events.
METHODS We included 1726 asymptomatic individuals (1018
men, 708 women, age 57.7 +/- 13.3 years) referred for a cardiological
examination. Coronary calcifications were determined with the
Imatron C 150 XP electron beam computed tomography scanner. For
quantification of coronary calcifications, we calculated the Agatston
score. Over a mean observation period of 40.3 +/- 7.3 months we
registered the event rate for cardiac death (CD) and myocardial
infarction (MI).
RESULTS The Agatston score in patients who died of CD (n
= 65) or had an MI (n = 114) was significantly higher compared
with those without cardiac events (458 +/- 228 vs 206 +/- 201,
P < .01). An Agatston score above the 75th percentile was associated
with a significantly higher annualized event rate for MI (3.6%
vs 1.6%, P < .05) and for CD (2.2% vs 0.9%) compared with patients
with scores below the 75th percentile. No cardiac events were
observed in patients where coronary calcifications could be excluded.
CONCLUSIONS By determination of coronary calcifications,
patients at risk for future MI and CD could be identified within
an asymptomatic population independent of concomitant risk factors.
At the same time, future cardiovascular events could be excluded
in patients without coronary calcifications.
Mean
Agatston score, SD, and range depending on cardiovascular risk
factors.
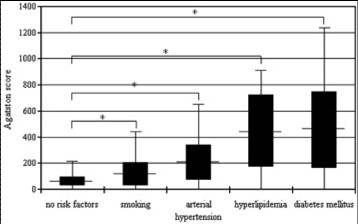
*
significant difference (P < .05) compared with the scores of
the patient group without cardiovascular risk factors
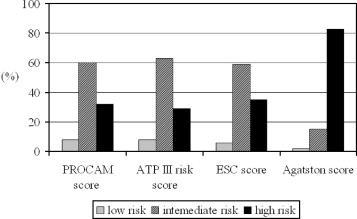
Risk
stratification according to ATP III risk score, PROCAM score,
Agatston score, and ESC score
in patients with nonfatal MI or CD.
|
|
|
|
|
|
RISCHIO
DI INFARTO MIOCARDIOCO E ICTUS: AGGIORNAMENTO DEL PROCAM RISK SCORE
[ASSESSING RISK OF MYOCARDIAL INFARCTION AND STROKE:
NEW DATA FROM THE PROSPECTIVE CARDIOVASCULAR MÜNSTER (PROCAM)
STUDY. Eur J Clin Invest. 2007 Dec;37(12):925-32]
ABSTRACT
OBJECTIVES Based on the data of the Prospective Cardiovascular
Münster (PROCAM) study, a prospective study of men and women
at work in the north-west of Germany, we aimed (i) to develop a
refined scoring scheme for calculating the risk of acute coronary
events among adult and elderly men and women; and (ii) to generate
a new scoring scheme for calculating the risk of ischaemic stroke
or transient ischaemic attack (TIA).
METHODS The coronary risk score was derived from a Weibull
function using data from 18 460 men and 8515 women who were recruited
before 1996 and had a mean follow-up period of 12+/-6 years. The
stroke score was derived using a Cox proportional hazards model
using data of 5905 men and 2225 women aged 35-65 years with at least
10 years of unbroken follow-up.
RESULTS The coronary risk score was based on 511 major coronary
events, 462 (168 fatal, 294 non-fatal) in men and 49 (18 fatal,
31 non-fatal) in women and included the risk factors LDL cholesterol,
HDL cholesterol, systolic blood pressure, smoking status, triglycerides
and diabetes mellitus status. It was accurate in both sexes over
an age range from 20 to 75 years with an area under the receiver-operating
characteristics (ROC) curve of 0.82. The stroke score was based
on 85 cerebral ischaemic events (21 TIAs, 64 ischaemic strokes)
and included the risk factors age, sex, diabetes mellitus status,
smoking status and systolic blood pressure. It had an area under
the ROC curve of 0.78 and identified a high-risk group comprising
only 4% of the study population that contained 31% of all cerebral
ischaemic events.
CONCLUSION Both new PROCAM risk scores provide simple and
effective ways to assess the risk of acute coronary events and ischaemic
stroke in the general population and will improve the ability of
physicians to target measures in an effort to prevent these potentially
devastating conditions.
|
|
|
|
|
|
EFFETTI
DELLA COMBINAZIONE ATTIVITÀ FISICA-CONSUMO DI ALCOL SULLA
MORTALITÀ PER ISCHEMIA CARDIACA E PER TUTTE LE CAUSE
[THE COMBINED INFLUENCE OF LEISURE-TIME PHYSICAL ACTIVITY AND
WEEKLY ALCOHOL INTAKE ON FATAL ISCHAEMIC HEART DISEASE AND ALL-CAUSE
MORTALITY. Eur Heart J, pubblicato on line il 9 gennaio 2008]
ABSTRACT
AIMS To determine the combined influence of leisure-time
physical activity and weekly alcohol intake on the risk of subsequent
fatal ischaemic heart disease (IHD) and all-cause mortality.
METHODS AND RESULTS Prospective cohort study of 11 914 Danes
aged 20 years or older and without pre-existing IHD. During 20 years
of follow-up, 1242 cases of fatal IHD occurred and 5901 died from
all causes. Within both genders, being physically active was associated
with lower hazard ratios (HR) of both fatal IHD and all-cause mortality
than being physically inactive. Further, weekly alcohol intake was
inversely associated with fatal IHD and had a U-shaped association
with all-cause mortality. Within level of physical activity, non-drinkers
had the highest HR of fatal IHD, whereas both non-drinkers and heavy
drinkers had the highest HR of all-cause mortality. Further, the
physically inactive had the highest HR of both fatal IHD and all-cause
mortality within each category of weekly alcohol intake. Thus, the
HR of both fatal IHD and all-cause mortality were low among the
physically active who had a moderate alcohol intake.
CONCLUSION Leisure-time physical activity and a moderate
weekly alcohol intake are both important to lower the risk of fatal
IHD and all-cause mortality.
|
|
|
|
|
|
ATTIVITÀ
FISICA ED ETÀ BIOLOGICA
[THE ASSOCIATION BETWEEN PHYSICAL ACTIVITY IN
LEISURE TIME AND LEUKOCYTE TELOMERE LENGTH. Arch Intern Med 2008;
168:154-158]
ABSTRACT
BACKGROUND Physical inactivity is an important risk factor
for many aging-related diseases. Leukocyte telomere dynamics (telomere
length and age-dependent attrition rate) are ostensibly a biological
indicator of human aging. We therefore tested the hypothesis that
physical activity level in leisure time (over the past 12 months)
is associated with leukocyte telomere length (LTL) in normal healthy
volunteers.
METHODS We studied 2401 white twin volunteers, comprising
2152 women and 249 men, with questionnaires on physical activity
level, smoking status, and socioeconomic status. Leukocyte telomere
length was derived from the mean terminal restriction fragment
length and adjusted for age and other potential confounders.
RESULTS Leukocyte telomere length was positively associated
with increasing physical activity level in leisure time (P <
.001); this association remained significant after adjustment
for age, sex, body mass index, smoking, socioeconomic status,
and physical activity at work. The LTLs of the most active subjects
were 200 nucleotides longer than those of the least active subjects
(7.1 and 6.9 kilobases, respectively; P = .006). This finding
was confirmed in a small group of twin pairs discordant for physical
activity level (on average, the LTL of more active twins was 88
nucleotides longer than that of less active twins; P = .03).
CONCLUSIONS A sedentary lifestyle (in addition to smoking,
high body mass index, and low socioeconomic status) has an effect
on LTL and may accelerate the aging process. This provides a powerful
message that could be used by clinicians to promote the potentially
antiaging effect of regular exercise.
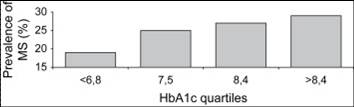
Mean
telomere length and standard error bars by physical activity level
in leisure time.
BMI
body mass index; kb kilobases; SES socioeconomic status
|
|
|
|
|
|
FITNESS
E MORTALITÀ
[EXERCISE CAPACITY AND MORTALITY IN BLACK AND
WHITE MEN. Circulation, pubblicato on line il 22 gennaio 2008]
ABSTRACT
BACKGROUND Exercise capacity is inversely related to mortality
risk in healthy individuals and those with cardiovascular diseases.
This evidence is based largely on white populations, with little
information available for blacks.
METHODS AND RESULTS We assessed the association between exercise
capacity and mortality in black (n=6749; age, 58±11 years)
and white (n=8911; age, 60±11 years) male veterans with and
without cardiovascular disease who successfully completed a treadmill
exercise test at the Veterans Affairs Medical Centers in Washington,
DC, and Palo Alto, Calif. Fitness categories were based on peak
metabolic equivalents (METs) achieved. Subjects were followed up
for all-cause mortality for 7.5±5.3 years. Among clinical
and exercise test variables, exercise capacity was the strongest
predictor of risk for mortality. The adjusted risk was reduced by
13% for every 1-MET increase in exercise capacity (hazard ratio,
0.87; 95% confidence interval, 0.86 to 0.88; P<0.001). Compared
with those who achieved <5 METs, the mortality risk was 50% lower
for those with an exercise capacity of 7.1 to 10 METs (hazard ratio,
0.51; 95% confidence interval, 0.47 to 0.56; P<0.001) and 70%
lower for those achieving >10 METs (hazard ratio, 0.31; 95% confidence
interval, 0.26 to 0.36; P<0.001). The findings were similar for
those with and without cardiovascular disease and for both races.
CONCLUSIONS Exercise capacity is a strong predictor of all-cause
mortality in blacks and whites. The relationship was inverse and
graded, with a similar impact on mortality outcomes for both blacks
and whites.
|
|
|
|
|
|
ATTIVITÀ
FISICA E DIMINUZIONE DEL RISCHIO DI EVENTI CARDIOVASCOLARI
[PHYSICAL ACTIVITY AND REDUCED RISK OF CARDIOVASCULAR
EVENTS. POTENTIAL MEDIATING MECHANISMS. Circulation 2007; 116: 2110-2118]
ABSTRACT
LEARNING OBJECTIVE At the conclusion, the learner will identify
the changes in CVD risk factors associated with increased physical
activity in the Women's Health Study.
STUDY QUESTION Higher levels of physical activity are associated
with fewer cardiovascular disease (CVD) events. What are the several
CV risk factors that may mediate this effect?
METHODS In a prospective study of 27,055 apparently healthy
women participating in the Women's Health Study (WHS), the following
were measured: baseline levels of hemoglobin A1c, total cholesterol,
low-density lipoprotein cholesterol, high-density lipoprotein cholesterol,
lipoprotein (a) and apolipoprotein A-1 and B-100, creatinine, homocysteine,
and inflammatory/hemostatic biomarkers (high-sensitivity C-reactive
protein, fibrinogen, soluble intracellular adhesion molecule-1)
and self-reported physical activity, weight, height, hypertension,
and diabetes. Mean follow-up was 10.9 ± 1.6 years, and 979
incident CVD events occurred.
RESULTS The risk of CVD decreased linearly with higher levels
of activity (p for linear trend <0.0001). Using the reference
group of <200 kcal/wk of activity yielded age- and treatment-adjusted
relative risk reductions associated with 200-599, 600-1499, and
>=1500 kcal/wk of 27%, 32%, and 41% respectively. Differences
in known risk factors explained a large proportion (59.0%) of the
observed inverse association. When sets of risk factors were examined,
inflammatory/hemostatic biomarkers made the largest contribution
to lower risk (32.6%), followed by blood pressure (27.1%). Novel
lipids contributed less than standard lipids (15.5% and 19.1%, respectively).
Smaller contributions were attributed to body mass index (10.1%)
and hemoglobin A1c/diabetes (8.9%), whereas homocysteine and creatinine
had negligible effects (<1%).
CONCLUSIONS The inverse association between physical activity
and CVD risk is mediated in substantial part by known risk factors,
particularly inflammatory/hemostatic factors and blood pressure.
PERSPECTIVE Participating women in the WHS were randomized
to placebo versus aspirin and/or vitamin E, and were followed for
CV outcomes. It is unlikely there was a bias regarding outcome measures,
but much was self-reported and these were predominantly healthy
professionals. The findings are consistent with observational studies,
and repeat the message that moderate exercise, as little as one-half
hour 3 days a week, provides highly significant benefits, and more
is better. That nearly one-third of the benefit to lower CV risk
is not measured in the clinic is an important message for patients
who would focus on weight and lipids.
|
|
|
|
|
|
ESERCIZIO
FISICO E SINDROME METABOLICA
[EXERCISE TRAINING AMOUNT AND INTENSITY ON METABOLIC
SYNDROME (FROM STUDIES OF A TARGETED RISK REDUCTION INTERVENTION
THROUGH DEFINED EXERCISE).Am J Cardiol 2007; 100:1759-1766]
ABSTRACT
Although exercise improves individual risk factors for metabolic
syndrome (MS), there is little research on the effect of exercise
on MS as a whole. The objective of this study was to determine how
much exercise is recommended to decrease the prevalence of MS. Of
334 subjects randomly assigned, 227 finished and 171 (80 women,
91 men) had complete data for all 5 Adult Treatment Panel III-defined
MS risk factors and were included in this analysis.
Subjects were randomly assigned to a 6-month control or 1 of 3 eight-month
exercise training groups of (1) low amount/moderate intensity (equivalent
to walking approximately 19 km/week), (2) low amount/vigorous intensity
(equivalent to jogging approximately 19 km/week), or (3) high amount/vigorous
intensity (equivalent to jogging approximately 32 km/week).
The low-amount/moderate-intensity exercise prescription improved
MS relative to inactive controls (p <0.05). However, the same
amount of exercise at vigorous intensity was not significantly better
than inactive controls, suggesting that lower-intensity exercise
may be more effective in improving MS. The high-amount/vigorous-intensity
group improved MS relative to controls (p <0.0001), the low-amount/vigorous-intensity
group (p = 0.001), and the moderate-intensity group (p = 0.07),
suggesting an exercise-dose effect.
In conclusion, a modest amount of moderate-intensity exercise in
the absence of dietary changes significantly improved MS and thus
supported the recommendation that adults get 30 minutes of moderate-intensity
exercise every day. A higher amount of vigorous exercise had greater
and more widespread benefits. Finally, there was an indication that
moderate-intensity may be better than vigorous-intensity exercise
for improving MS.
|
|
|
|
|
|
ANNO
DI NASCITA, ETA' E FATTORI DI RISCHIO CARDIOVASCOLARI
[CHANGES OF CARDIOVASCULAR RISK FACTORS AND
THEIR IMPLICATIONS IN SUBSEQUENT BIRTH COHORTS OF OLDER ADULTS
IN GERMANY: A LIFE COURSE APPROACH. Eur J Cardiovasc Prev Rehabil
2007; 14:809-814]
ABSTRACT
BACKGROUND To examine lifetime patterns of cardiovascular
risk factors and their implications in subsequent birth cohorts
of older adults in Germany, who experienced very different political
and socioeconomic conditions at various phases of their lives.
DESIGN AND METHODS Participants of the ESTHER study, a
statewide cohort study conducted in Saarland, Germany, were categorized
into four birth cohorts: 1925-1934, 1935-1939, 1940-1944, 1945-1952.
At baseline, lifetime history of body weight, physical activity,
smoking and drinking habits, and of physician-diagnosed diabetes
mellitus were documented. The average BMI, the average number
of hours of physical activity, prevalence of smoking and alcohol
consumption between ages 20 and 50 years were assessed. The relative
risks of a first diagnosis of diabetes mellitus before or at the
age of 50 years by birth cohorts were assessed by multiple logistic
regressions controlling for education and BMI at the age of 20.
RESULTS For both men and women, later birth cohorts had
considerably worse lifestyle profiles. The frequency of diabetes
mellitus up to the age of 50 years was much higher in the later
than in the earlier cohorts. The increase was more pronounced
among men than among women.
CONCLUSION Women and men reaching old age in the forthcoming
years have more unfavourable lifetime risk factor profiles than
earlier birth cohorts. These patterns might have substantial implications
for the future burden of chronic disease.
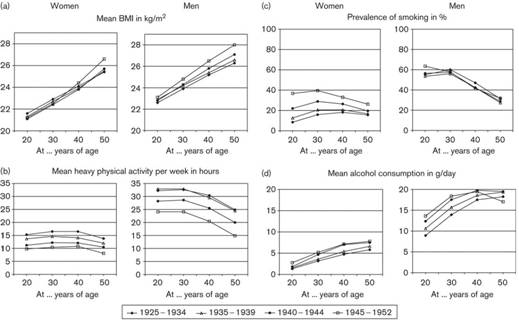
Distribution
of lifestyle factors as different stages of life for the four
ESTHER birth cohorts, stratified for gender.
|
|
|
|
| |
QUALITÀ
NELLA CURA DEL DIABETE E RISCHIO DI CVD
[QUALITY OF DIABETES CARE PREDICTS THE DEVELOPMENT
OF CARDIOVASCULAR EVENTS: RESULTS OF THE QUED STUDY. Nutr Metab
Cardiovasc Dis 2008; 18:57-65]
ABSTRACT
BACKGROUND AND AIM In the context of the QuED Study we assessed
whether a quality of care summary score was able to predict the
development of cardiovascular (CV) events in patients with type
2 diabetes.
METHODS AND RESULTS The score was calculated using process
and intermediate outcome indicators (HbA1c, blood pressure, low-density
lipoprotein cholesterol, microalbuminuria) and ranged from 0 to
40. Overall, 3235 patients were enrolled, of whom 492 developed
a CV event after a median follow-up of 5 years. The incidence rate
(per 1000 person-years) of CV events was 62.4 in patients with a
score <=10, 54.8 in those with a score between 15 and 20, and
39.8 in those with a score >20. In adjusted multilevel regression
models, the risk to develop a CV event was 89% greater in patients
with a score of <=10 (rate ratio [RR] = 1.89; 95% confidence
interval [CI] 1.43-2.50) and 43% higher in those with a score between
10 and 20 (RR = 1.43; 95% CI 1.14-1.79), as compared to those with
a score >20. A difference between centers of 5 points in the
mean quality score was associated with a difference of 16% in CV
event risk (RR = 0.84; 95% CI 0.72-0.98).
CONCLUSION Our study documented for the first time a close
relationship between a score of quality of diabetes care and long-term
outcomes.
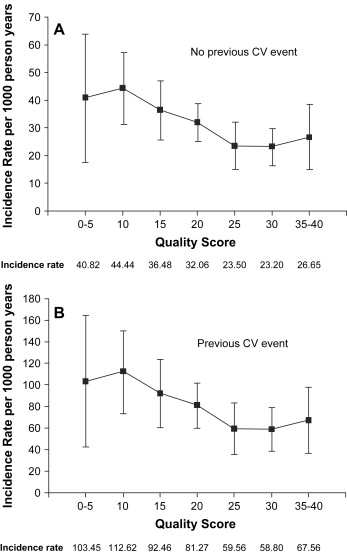
Quality
of care scoring system
| Quality
of care indicator |
Scoring
|
| HbA1c
measurement < 1/year |
5
|
| HbA1c
>= 8.0% |
0
|
| HbA1c
< 8.0% |
10
|
| Blood
pressure measurement < 1/year |
5
|
| Blood
pressure values >= 140/90 mmHg, irrespective of treatment
|
0
|
| Blood
pressure values < 140/90 mmHg |
10
|
| Lipid
profile measurement < 1/year |
5
|
| LDL
cholesterol >= 3.37 mmol/L (130 mg/dL) irrespective of
treatment |
0
|
| LDL
cholesterol < 3.37 mmol/L (130 mg/dL) |
10
|
| MA
measurement < 1/year |
5
|
| Not
treated with ACE-inhibitors despite the presence of MA |
0
|
| Treated
with ACE-inhibitors in the presence of MA or MA absent |
10
|
| Score
range |
0-40
|
Hb
hemoglobin; LDL low-density lipoprotein; MA microalbuminuria;
ACE angiotensin-converting enzyme
Incidence rates and 95% confidence intervals for any CV event
by quality of care score classes,
adjusted for age and diabetes duration.
Incidence rates are expressed as number of events per 1000 person-years
and are reported separately
for patients without previous CV event and for patients with prior
CV event.
|
|
|
|
| |
CARENZA
DI VITAMINA D E RISCHIO DI CVD
[VITAMIN D DEFICIENCY AND RISK OF CARDIOVASCULAR
DISEASE. Circulation, pubblicato on line il 7 gennaio 2008]
ABSTRACT
BACKGROUND Vitamin D receptors have a broad tissue distribution
that includes vascular smooth muscle, endothelium, and cardiomyocytes.
A growing body of evidence suggests that vitamin D deficiency may
adversely affect the cardiovascular system, but data from longitudinal
studies are lacking.
METHODS AND RESULTS We studied 1739 Framingham Offspring
Study participants (mean age 59 years; 55% women; all white) without
prior cardiovascular disease. Vitamin D status was assessed by measuring
25-dihydroxyvitamin D (25-OH D) levels. Prespecified thresholds
were used to characterize varying degrees of 25-OH D deficiency
(<15 ng/mL, <10 ng/mL). Multivariable Cox regression models
were adjusted for conventional risk factors. Overall, 28% of individuals
had levels <15 ng/mL, and 9% had levels <10 ng/mL. During
a mean follow-up of 5.4 years, 120 individuals developed a first
cardiovascular event. Individuals with 25-OH D <15 ng/mL had
a multivariable-adjusted hazard ratio of 1.62 (95% confidence interval
1.11 to 2.36, P=0.01) for incident cardiovascular events compared
with those with 25-OH D 15 ng/mL. This effect was evident in participants
with hypertension (hazard ratio 2.13, 95% confidence interval 1.30
to 3.48) but not in those without hypertension (hazard ratio 1.04,
95% confidence interval 0.55 to 1.96). There was a graded increase
in cardiovascular risk across categories of 25-OH D, with multivariable-adjusted
hazard ratios of 1.53 (95% confidence interval 1.00 to 2.36) for
levels 10 to <15 ng/mL and 1.80 (95% confidence interval 1.05
to 3.08) for levels <10 ng/mL (P for linear trend=0.01). Further
adjustment for C-reactive protein, physical activity, or vitamin
use did not affect the findings.
CONCLUSIONS Vitamin D deficiency is associated with incident
cardiovascular disease. Further clinical and experimental studies
may be warranted to determine whether correction of vitamin D deficiency
could contribute to the prevention of cardiovascular disease.
|
|
|
|
| |
BASSE
CONCENTRAZIONI DI VITAMINA D E PRESSIONE ARTERIOSA
[SERUM 25-HYDROXYVITAMIN D, ETHNICITY, AND BLOOD
PRESSURE IN THE THIRD NATIONAL HEALTH AND NUTRITION EXAMINATION
SURVEY. Am J Hyperten 2007; 20:713-719]
ABSTRACT
BACKGROUND Populations with low vitamin D status, such as
blacks living in the US or UK, have increased blood pressure (BP)
compared with whites. We analyzed the association between serum
25-hydroxyvitamin D (25OHD) and BP to determine whether low 25OHD
explains any of the increased BP in blacks.
METHODS The Third US National Health and Nutrition Examination
Survey (NHANES III) is a cross-sectional survey representative of
the US civilian population during 1988 to 1994. Analyses were restricted
to 12,644 people aged > or =20 years with measurements of BP
and 25OHD, after excluding those on hypertensive medication.
RESULTS Adjusted mean serum 25OHD was lowest in non-Hispanic
blacks (49 nmol/L), intermediate in Mexican Americans (68 nmol/L),
and highest in non-Hispanic whites (79 nmol/L). When participants
were divided into 25OHD quintiles, mean (standard error) systolic
BP was 3.0 (0.7) mm Hg lower (P = .0004) and diastolic BP was 1.6
(0.6) mm Hg lower (P = .011) for participants in the highest quintile
(25OHD > or =85.7 nmol/L) compared with the lowest (25OHD <
or =40.4 nmol/L), adjusting for age, sex, ethnicity, and physical
activity. Further adjustment for body mass index (BMI) weakened
the inverse association between 25OHD and BP, which remained significant
for systolic BP (P < .05). The inverse association between 25OHD
and systolic BP was stronger in participants aged > or =50 years
than younger (P = .021). Ethnic differences in 25OHD explained about
half of the increased hypertension prevalence in non-Hispanic blacks
compared with whites.
CONCLUSIONS Vitamin D status, which is amenable to intervention
by safely increasing sun exposure or vitamin D supplementation,
was associated inversely with BP in a large sample representative
of the US population.
|
|
|
|
| |
FATTORI
DI RISCHIO CARDIOVASCOLARI E TROMBOEMBOLISMO VENOSO
[CARDIOVASCULAR RISK FACTORS AND VENOUS THROMBOEMBOLISM:
A META-ANALYSIS. Circulation 2008; 117: 93-102]
ABSTRACT
BACKGROUND The concept that venous thromboembolism (VTE)
and atherosclerosis are 2 completely distinct entities has recently
been challenged because patients with VTE have more asymptomatic
atherosclerosis and more cardiovascular events than control subjects.
We performed a meta-analysis to assess the association between cardiovascular
risk factors and VTE.
METHODS AND RESULTS Medline and EMBASE databases were searched
to identify studies that evaluated the prevalence of major cardiovascular
risk factors in VTE patients and control subjects. Studies were
selected using a priori defined criteria, and each study was reviewed
by 2 authors who abstracted data on study characteristics, study
quality, and outcomes. Odds ratios or weighted means and 95% confidence
intervals (CIs) were then calculated and pooled using a random-effects
model. Statistical heterogeneity was evaluated through the use of
2 and I2 statistics. Twenty-one case-control and cohort studies
with a total of 63 552 patients met the inclusion criteria. Compared
with control subjects, the risk of VTE was 2.33 for obesity (95%
CI, 1.68 to 3.24), 1.51 for hypertension (95% CI, 1.23 to 1.85),
1.42 for diabetes mellitus (95% CI, 1.12 to 1.77), 1.18 for smoking
(95% CI, 0.95 to 1.46), and 1.16 for hypercholesterolemia (95% CI,
0.67 to 2.02). Weighted mean high-density lipoprotein cholesterol
levels were significantly lower in VTE patients, whereas no difference
was observed for total and low-density lipoprotein cholesterol levels.
Significant heterogeneity among studies was present in all subgroups
except for the diabetes mellitus subgroup. Higher-quality studies
were more homogeneous, and significant associations remained unchanged.
CONCLUSIONS Cardiovascular risk factors are associated with
VTE. This association is clinically relevant with respect to individual
screening, risk factor modification, and primary and secondary prevention
of VTE. Prospective studies should further investigate the underlying
mechanisms of this relationship.
|
|
|
|
| |
SINDROME
DELLE GAMBE SENZA RIPOSO E PATOLOGIA CARDIOVASCOLARE
[ASSOCIATION OF RESTLESS LEGS SYNDROME AND CARDIOVASCULAR
DISEASE IN THE SLEEP HEART HEALTH STUDY. Neurology 2008; 70:35-42]
ABSTRACT
OBJECTIVE We evaluated the cross-sectional association between
restless legs syndrome (RLS) and prevalent cardiovascular disease
(CVD) in a large community-based sample of middle-aged and elderly
subjects.
METHODS This is a cross-sectional observational study of
1,559 men and 1,874 women (mean age of 67.9 years) who were enrolled
in the Sleep Heart Health Study, a community-based study of the
cardiovascular consequences of sleep-disordered breathing. RLS was
defined by positive responses on a self-administered questionnaire
to the four diagnostic criteria, with symptoms occurring at least
five times per month and associated with at least moderate distress.
Coronary artery disease (CAD) was determined by self-report of doctor-diagnosed
angina, myocardial infarction, or coronary revascularization procedure.
Total CVD included CAD or history of physician-diagnosed stroke
or heart failure. The relation of RLS to prevalent CAD and CVD was
examined by multivariable logistic regression models
RESULTS RLS was present in 6.8% of women (n = 128) and 3.3%
of men (n = 51). After adjustment for age, sex, race, body mass
index, diabetes mellitus, systolic blood pressure, antihypertensive
medication use, total:high-density lipoprotein cholesterol ratio,
and smoking history, the ORs for CAD were 2.05 (95% CI 1.38 to 3.04)
and for CVD were 2.07 (1.43 to 3.00) for subjects with RLS compared
to those without RLS. The associations of RLS with CAD and CVD were
stronger in those with RLS symptoms at least 16 times per month
and were stronger in those with severe than in those with moderately
bothersome symptoms.
CONCLUSIONS Restless legs syndrome (RLS) is associated with
prevalent coronary artery disease and cardiovascular disease. This
association appears stronger in those with greater frequency or
severity of RLS symptoms.
|
|
|
|
| |
LIVELLI
DI PCR E FUTURA PATOLOGIA RENALE IN SOGGETTI SOVRAPPESO OD OBESI
SENZA DIABETE MELLITO NÉ IPERTENSIONE
[THE PREDICTIVE VALUE OF CRP LEVELS ON FUTURE
SEVERE RENAL DISEASE IN OVERWEIGHT AND OBESE SUBJECTS WITHOUT DIABETES
MELLITUS AND HYPERTENSION. Am J Med Sci 2007; 334:444-451]
ABSTRACT
BACKGROUND Obesity and related disorders have a high prevalence
all over the world. Increased C-reactive protein (CRP) value in
obese individuals and its potential adverse effects have been reported.
Here we have investigated the relationship between CRP levels and
renal functions in nondiabetic, nonhypertensive, overweight, and
obese individuals. The aim of this study was to evaluate the predictive
value of CRP levels on future severe renal disease.
METHODS One hundred sixty individuals were included in the
study. They were grouped as normal weight, overweight, and obese.
Anthropometric measurements, renal function tests, and serum hsCRP
values were obtained. Mean values were compared and correlation
analysis was performed.
RESULTS Significant differences were detected between the
groups according to body mass index, waist circumference (WC), and
body fat percentage. There was a significant difference with respect
to creatinine clearance (CC). Difference in the mean urinary albumin
excretion (UAE) was significant between normal-weight and overweight
subjects. There was a linear increase in serum CRP values in parallel
to the increase in body weight; mean values were significant between
groups. A positive correlation was detected between CC and body
mass index and WC, and there were significant correlations between
CRP and anthropometric measurements, CC and UAE.
CONCLUSIONS This study showed that increased CRP levels in
nondiabetic, nonhypertensive, overweight, and obese individuals
could possibly associated with impaired renal functions that might
be originating from endothelial dysfunction. Determination of cutoff
levels of CRP, as in cardiovascular diseases, may be useful for
early estimation and prevention of renal diseases.
|
|
|
|
| |
INDICE
DI MASSA CORPOREA E INCIDENZA DI CANCRO E MORTALITÀ NELLE
DONNE
[CANCER INCIDENCE AND MORTALITY IN RELATION TO
BODY MASS INDEX IN THE MILLION WOMEN STUDY: COHORT STUDY. BMJ 2007;
335:1134]
ABSTRACT
OBJECTIVE To examine the relation between body mass index
(kg/m2) and cancer incidence and mortality.
DESIGN Prospective cohort study.
PARTICIPANTS 1.2 million UK women recruited into the Million
Women Study, aged 50-64 during 1996-2001, and followed up, on average,
for 5.4 years for cancer incidence and 7.0 years for cancer mortality.
MAIN OUTCOME MEASURES Relative risks of incidence and mortality
for all cancers, and for 17 specific types of cancer, according
to body mass index, adjusted for age, geographical region, socioeconomic
status, age at first birth, parity, smoking status, alcohol intake,
physical activity, years since menopause, and use of hormone replacement
therapy.
RESULTS 45 037 incident cancers and 17 203 deaths from cancer
occurred over the follow-up period. Increasing body mass index was
associated with an increased incidence of endometrial cancer (trend
in relative risk per 10 units=2.89, 95% confidence interval 2.62
to 3.18), adenocarcinoma of the oesophagus (2.38, 1.59 to 3.56),
kidney cancer (1.53, 1.27 to 1.84), leukaemia (1.50, 1.23 to 1.83),
multiple myeloma (1.31, 1.04 to 1.65), pancreatic cancer (1.24,
1.03 to 1.48), non-Hodgkin's lymphoma (1.17, 1.03 to 1.34), ovarian
cancer (1.14, 1.03 to 1.27), all cancers combined (1.12, 1.09 to
1.14), breast cancer in postmenopausal women (1.40, 1.31 to 1.49)
and colorectal cancer in premenopausal women (1.61, 1.05 to 2.48).
In general, the relation between body mass index and mortality was
similar to that for incidence. For colorectal cancer, malignant
melanoma, breast cancer, and endometrial cancer, the effect of body
mass index on risk differed significantly according to menopausal
status.
CONCLUSIONS Increasing body mass index is associated with
a significant increase in the risk of cancer for 10 out of 17 specific
types examined. Among postmenopausal women in the UK, 5% of all
cancers (about 6000 annually) are attributable to being overweight
or obese. For endometrial cancer and adenocarcinoma of the oesophagus,
body mass index represents a major modifiable risk factor; about
half of all cases in postmenopausal women are attributable to overweight
or obesity.
|
|
|
|
| |
CIRFCONFERENZA
VITA, DIABETE E MALATTIE CARDIOVASCOLARI
[DOES WAIST CIRCUMFERENCE PREDICT DIABETES AND
CARDIOVASCULAR DISEASE BEYOND COMMONLY EVALUATED CARDIOMETABOLIC
RISK FACTORS? Diabetes Care. 2007;30:3105-9]
ABSTRACT
OBJECTIVE While the measurement of waist circumference
(WC) is recommended in current clinical guidelines, its clinical
utility was questioned in a recent consensus statement. In response,
we sought to determine whether WC predicts diabetes and cardiovascular
disease (CVD) beyond that explained by BMI and commonly obtained
cardiometabolic risk factors including blood pressure, lipoproteins,
and glucose.
RESEARCH DESIGN AND METHODS Subjects consisted of 5,882
adults from the 1999-2004 National Health and Nutrition Examination
Survey, which is nationally representative and cross-sectional.
Subjects were grouped into sex-specific WC and BMI tertiles. Blood
pressure, triglycerides, LDL and HDL cholesterol, and glucose
were categorized using standard clinical thresholds. Logistic
regression analyses were used to calculate the odds for diabetes
and CVD according to WC tertiles.
RESULTS After controlling for basic confounders, the medium
and high WC tertiles were more likely to have diabetes and CVD
compared with the low WC tertile (P < 0.05). After inclusion
of BMI and cardiometabolic risk factors in the regression models,
the magnitude of the odds ratios were attenuated (i.e., for diabetes
the magnitude decreased from 6.54 to 5.03 for the high WC group)
but remained significant in the medium and high WC tertiles for
the prediction of diabetes, though not for CVD.
CONCLUSIONS WC predicted diabetes, but not CVD, beyond
that explained by traditional cardiometabolic risk factors and
BMI. The findings lend critical support for the recommendation
that WC be a routine measure for identification of the high-risk,
abdominally obese patient.
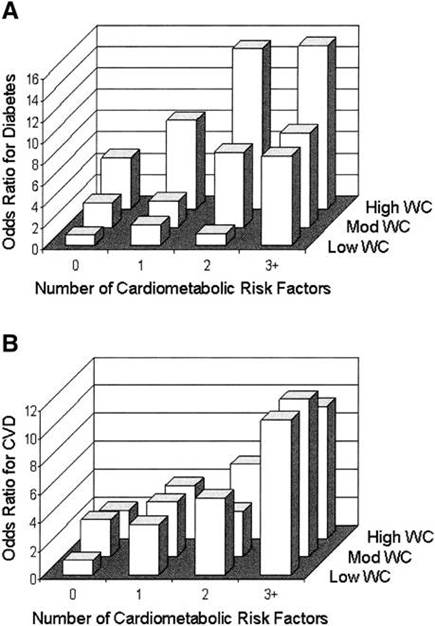
ORs
for diabetes (A) and CVD (B) according to WC x metabolic risk
factor groups.
Both WC and metabolic risk factor groups were independent
predictors of diabetes (Ptrend < 0.001).
[WAIST
CIRCUMFERENCE THRESHOLDS PROVIDE AN ACCURATE AND WIDELY APPLICABLE
METHOD FOR THE DISCRIMINATION OF DIABETES. Diabetes Care. 2007;30:3116-8]
ABSTRACT
Excess weight, particularly central obesity, is recognized to
be a major determinant of diabetes risk in all populations, with
the magnitude of the association reported as being stronger in
Asians than whites (1-3). Consequently, indicators of overweight
have been incorporated into several guidelines for the early identification
of individuals with type 2 diabetes (4). However, the anthropometric
cut points for different ethnic groups have been determined in
various ways, leading to uncertainty about their applicability
to diabetes screening. Here, we clarify current uncertainty regarding
ethnic differences in the relationship between overweight and
diabetes and whether there is a single measure of overweight that
can be determined routinely and applied universally in clinical
practice to facilitate earlier detection of diabetes in the general
population.
|
|
|
|
| |
ALIMENTAZIONE
E SINDROME METABOLICA
[DIETARY INTAKE AND THE DEVELOPMENT OF THE METABOLIC
SYNDROME. Circulation, pubblicato on line il 22 gennaio 2008]
ABSTRACT
BACKGROUND The role of diet in the origin of metabolic syndrome
(MetSyn) is not well understood; thus, we sought to evaluate the
relationship between incident MetSyn and dietary intake using prospective
data from 9514 participants (age, 45 to 64 years) enrolled in the
Atherosclerosis Risk in Communities (ARIC) study.
METHODS AND RESULTS Dietary intake was assessed at baseline
via a 66-item food frequency questionnaire. We used principal-components
analysis to derive "Western" and "prudent" dietary
patterns from 32 food groups and evaluated 10 food groups used in
previous studies of the ARIC cohort. MetSyn was defined by American
Heart Association guidelines. Proportional-hazards regression was
used. Over 9 years of follow-up, 3782 incident cases of MetSyn were
identified. After adjustment for demographic factors, smoking, physical
activity, and energy intake, consumption of a Western dietary pattern
(Ptrend=0.03) was adversely associated with incident MetSyn. After
further adjustment for intake of meat, dairy, fruits and vegetables,
refined grains, and whole grains, analysis of individual food groups
revealed that meat (Ptrend<0.001), fried foods (Ptrend=0.02),
and diet soda (Ptrend=< 0.001) also were adversely associated
with incident MetSyn, whereas dairy consumption (Ptrend=0.006) was
beneficial. No associations were observed between incident MetSyn
and a prudent dietary pattern or intakes of whole grains, refined
grains, fruits and vegetables, nuts, coffee, or sweetened beverages.
CONCLUSIONS These prospective findings suggest that consumption
of a Western dietary pattern, meat, and fried foods promotes the
incidence of MetSyn, whereas dairy consumption provides some protection.
The diet soda association was not hypothesized and deserves further
study.
|
|
|
|
| |
SINDROME
METABOLICA E RISCHIO DI ICTUS ISCHEMICO
[METABOLIC SYNDROME AND ISCHEMIC STROKE RISK:
NORTHERN MANHATTAN STUDY. Stroke 2008; 39:30-35]
ABSTRACT
BACKGROUND AND PURPOSE More than 47 million individuals in
the United States meet the criteria for the metabolic syndrome.
The relation between the metabolic syndrome and stroke risk in multiethnic
populations has not been well characterized.
METHODS As part of the Northern Manhattan Study, 3298 stroke-free
community residents were prospectively followed up for a mean of
6.4 years. The metabolic syndrome was defined according to guidelines
established by the National Cholesterol Education Program Adult
Treatment Panel III. Cox proportional-hazards models were used to
calculate hazard ratios (HRs) and 95% CIs for ischemic stroke and
vascular events (ischemic stroke, myocardial infarction, or vascular
death). The etiologic fraction estimates the proportion of events
attributable to the metabolic syndrome.
RESULTS More than 44% of the cohort had the metabolic syndrome
(48% of women vs 38% of men, P<0.0001), which was more prevalent
among Hispanics (50%) than whites (39%) or blacks (37%). The metabolic
syndrome was associated with increased risk of stroke (HR=1.5; 95%
CI, 1.1 to 2.2) and vascular events (HR=1.6; 95% CI, 1.3 to 2.0)
after adjustment for sociodemographic and risk factors. The effect
of the metabolic syndrome on stroke risk was greater among women
(HR=2.0; 95% CI, 1.3 to 3.1) than men (HR=1.1; 95% CI, 0.6 to 1.9)
and among Hispanics (HR=2.0; 95% CI, 1.2 to 3.4) compared with blacks
and whites. The etiologic fraction estimates suggest that elimination
of the metabolic syndrome would result in a 19% reduction in overall
stroke, a 30% reduction of stroke in women; and a 35% reduction
of stroke among Hispanics.
CONCLUSIONS The metabolic syndrome is an important risk factor
for ischemic stroke, with differential effects by sex and race/ethnicity.
|
|
|
|
| |
MARKER
DI POTENZIALE ATEROSCLEROSI E RISCHIO DI CHD IN PAZIENTI DIABETICI
O CON SINDROME METABOLICA
[NON-TRADITIONAL MARKERS OF ATHEROSCLEROSIS
POTENTIATE THE RISK OF CORONARY HEART DISEASE IN PATIENTS WITH
TYPE 2 DIABETES AND METABOLIC SYNDROME. Nutr Metab Cardiovasc
Dis 2008; 18:31-8]
ABSTRACT
BACKGROUND AND AIMS The aims of this study were to establish
the prevalence of metabolic syndrome (MS), in type 2 diabetes
mellitus (DM), according to National Cholesterol Education Program
Adult Treatment Panel III (NCEP ATP III) criteria, and to assess
the association of MS with other cardiovascular (CV) risk factors
in these patients.
METHODS AND RESULTS A cross-sectional study was conducted
in 1610 patients with type 2 DM. Glycated hemoglobin A1c (HbA1c),
total cholesterol, low-density lipoprotein cholesterol (LDL-C)
and high-density lipoprotein cholesterol (HDL-C), uric acid, fibrinogen,
creatinine, and albumin/creatinine ratios were measured. The risk
of coronary heart disease (CHD) was calculated using the UKPDS
Risk Engine.
Seventy percent of the diabetic population met the criteria for
MS; central obesity and hypertension were the most common criteria.
Subjects with MS had higher levels of HbA1c, LDL-C, non-HDL-C,
uric acid, and fibrinogen compared to patients without MS. Similarly,
microalbuminuria and a high triglyceride (Tg)/HDL-C ratio (a marker
of small LDL-C) occurred more frequently in patients with MS.
When patients with no history of CHD events were considered, mean
CHD risk was greater in those with, than those without, MS.
CONCLUSIONS MS is highly prevalent in type 2 DM and is
commonly associated with non-traditional CV risk factors. The
diagnosis of MS seems to confer additional CHD risk in patients
with type 2 diabetes.
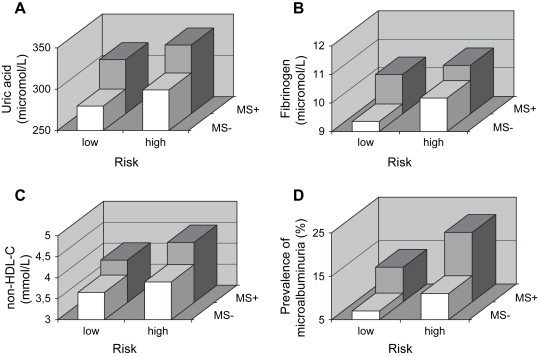
Number
and combination of traits of MS in type 2 diabetic patients.
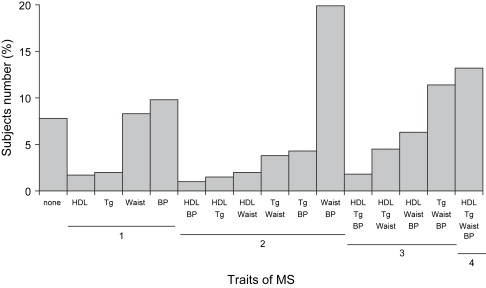
Prevalence of MS by HbA1c quartiles in type 2 diabetic patients
(p -trend > 0.0001).
Levels
of non-traditional cardiovascular risk factors (A, uric acid;
B, fibrinogen; C, non-HDL cholesterol; D, microalbuminuria)
in diabetics with (MS+) and without (MS-) metabolic syndrome in
relation to the estimated CHD risk
(high risk if >20%, low risk if <20%) (p < 0.0001).
|
|
|
|
| |
ANSIETÀ
E RISCHIO DI INFARTO MIOCARDICO ACUTO
[ANXIETY CHARACTERISTICS INDEPENDENTLY AND PROSPECTIVELY
PREDICT MYOCARDIAL INFARCTION IN MEN. THE UNIQUE CONTRIBUTION
OF ANXIETY AMONG PSYCHOLOGIC FACTORS. J Am Coll Cardiol 2008;
51:113-119]
ABSTRACT
OBJECTIVES This study investigated whether anxiety characteristics
independently predicted the onset of myocardial infarction (MI)
over an average of 12.4 years and whether this relationship was
independent of other psychologic variables and risk factors.
BACKGROUND Although several psychosocial factors have been
associated with risk for MI, anxiety has not been examined extensively.
Earlier studies also rarely addressed whether the association
between a psychologic variable and MI was specific and independent
of other psychosocial correlates.
METHODS Participants were 735 older men (mean age 60 years)
without a history of coronary disease or diabetes at baseline
from the Normative Aging Study. Anxiety characteristics were assessed
with 4 scales (psychasthenia, social introversion, phobia, and
manifest anxiety) and an overall anxiety factor derived from these
scales.
RESULTS Anxiety characteristics independently and prospectively
predicted MI incidence after controlling for age, education, marital
status, fasting glucose, body mass index, high-density lipoprotein
cholesterol, and systolic blood pressure in proportional hazards
models. The adjusted relative risk (95% confidence interval [CI])
of MI associated with each standard deviation increase in anxiety
variable was 1.37 (95% CI 1.12 to 1.68) for psychasthenia, 1.31
(95% CI 1.05 to 1.63) for social introversion, 1.36 (95% CI 1.10
to 1.68) for phobia, 1.42 (95% CI 1.14 to 1.76) for manifest anxiety,
and 1.43 (95% CI 1.17 to 1.75) for overall anxiety. These relationships
remained significant after further adjusting for health behaviors
(drinking, smoking, and caloric intake), medications for hypertension,
high cholesterol, and diabetes during follow-up and additional
psychologic variables (depression, type A behavior, hostility,
anger, and negative emotion).
CONCLUSIONS Anxiety-prone dispositions appear to be a robust
and independent risk factor of MI among older men.
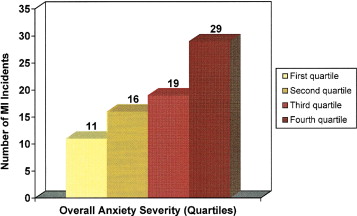
Number
of MI Incidents among participants in each anxiety quartile
(chi-square = 9.21; degrees of freedom = 3; p < 0.05)
|
|
|
|
| |
AUTOSTIMA
E RISCHIO DI OBESITÀ NELLE ADOLESCENTI
[SUBJECTIVE SOCIAL STATUS IN THE SCHOOL AND CHANGE
IN ADIPOSITY IN FEMALE ADOLESCENTS: FINDINGS FROM A PROSPECTIVE
COHORT STUDY. Arch Pediatr Adolesc Med. 2008; 162:23-8]
ABSTRACT
OBJECTIVE To determine whether subjective social standing
in school predicts a change in body mass index (BMI) in adolescent
girls during a 2-year period.
DESIGN Prospective cohort study.
SETTING Self-report questionnaires from a community-based
population of adolescent girls living across the United States from
1999 to 2001.
PARTICIPANTS Of 5723 girls aged 12 to 18 years participating
in the Growing Up Today Study (GUTS), adequate information was available
for 4446 (78%), who provided the analytic sample.
MAIN EXPOSURE Low subjective social status in the school.
MAIN OUTCOME MEASURES Change in BMI between 1999 and 2001
and multivariable odds ratio for a 2-U increase in BMI in girls
with low subjective social status in the school compared with girls
with higher subjective social status in the school.
RESULTS After adjusting for age, race/ethnicity, baseline
BMI, diet, television viewing, depression, global and social self-esteem,
menarche, height growth, mother's BMI, and pretax household income,
adolescent girls who placed themselves on the low end of the school
subjective social status scale had a 69% increased odds of having
a 2-unit increase in BMI (odds ratio, 1.69; 95% confidence interval,
1.10-2.60) during the next 2 years compared with other girls.
CONCLUSION Higher subjective social standing in school may
protect against gains in adiposity in adolescent girls.
|
|
|
|
| |
DEPRESSIONE
E ANSIETÀ E RISCHIO DI EVENTI CARDIACI IN PAZIENTI CON CORONAROPATIA
[DEPRESSION AND ANXIETY AS PREDICTORS OF 2-YEAR
CARDIAC EVENTS IN PATIENTS WITH STABLE CORONARY ARTERY DISEASE.
Arch Gen Psychiatry 2008; 65:62-71]
ABSTRACT
CONTEXT Anxiety and depression are associated with mechanisms
that promote atherosclerosis. Most recent studies of emotional disturbances
in coronary artery disease (CAD) have focused on depression only.
OBJECTIVE To assess the 2-year cardiac prognostic importance
of the DSM-IV-based diagnoses of major depressive disorder (MDD)
and generalized anxiety disorder (GAD) and self-report measures
of anxiety and depression and their co-occurrence.
DESIGN, SETTING, AND PATIENTS Two-year follow-up of 804 patients
with stable CAD (649 men) assessed using the Beck Depression Inventory
II (BDI-II), the anxiety subscale of the Hospital Anxiety and Depression
Scale (HADS-A), and the Structured Clinical Interview for DSM-IV
(masked to self-reports) 2 months after acute coronary syndromes.
MAIN OUTCOME MEASURES Major adverse cardiac events (MACEs)
(cardiac death, myocardial infarction, cardiac arrest, or nonelective
revascularization) in the 2 years after baseline.
RESULTS Of the 804 patients, 57 (7.1%) met the criteria for
MDD and 43 (5.3%) for GAD (11 [1.4%] had comorbidity); 220 (27.4%)
had elevated BDI-II scores (> or = 14), and 333 (41.4%) had elevated
HADS-A scores (> or = 8), with 21.1% overlap. MDD (odds ratio
[OR], 2.85; 95% confidence interval [CI], 1.62-5.01), GAD (OR, 2.09;
95% CI, 1.08-4.05), elevated BDI-II (OR, 1.75; 95% CI, 1.21-2.54),
elevated HADS-A score (OR, 1.67; 95% CI, 1.18-2.37), and continuous
standardized scores on the BDI-II (OR, 1.34; 95% CI, 1.11-1.62)
and the HADS-A (OR, 1.38; 95% CI, 1.16-1.63) all predicted MACEs.
After covariate control, only the P value associated with the continuous
BDI-II score increased to above .10. Most of the risk associated
with elevated symptoms was in patients with psychiatric disorders.
However, patients with comorbid MDD and GAD or elevated anxiety
and depression symptoms were not at greater MACE risk than those
with only 1 factor.
CONCLUSION Anxiety and depression predict greater MACE risk
in patients with stable CAD, supporting future research into common
genetic, environmental, and pathophysiologic pathways and treatments.
|
|
|
|
| |
FATTORI
DI RISCHIO CARDIOVASCOLARE NEI SOGGETTI CON ARTRITE REUMATOIDE
[CARDIOVASCULAR RISK FACTORS DIFFER IN MAGNITUDE
IN RHEUMATOID ARTHRITIS PATIENTS. Ann Rheum Dis 2008;67:64-69]
ABSTRACT
OBJECTIVE To compare the frequency of traditional cardiovascular
(CV) risk factors in rheumatoid arthritis (RA) compared to non-RA
subjects, and examine their impact on the risk of developing selected
CV events (myocardial infarction (MI), heart failure (HF) and
CV death) in these two groups.
METHODS We examined a population-based incidence cohort
of subjects with RA (defined according to the 1987 American College
of Rheumatology criteria), and an age- and sex-matched non-RA
cohort. All subjects were followed longitudinally through their
complete community medical records, until death, migration, or
1 January 2001. Clinical CV risk factors and outcomes were defined
using validated criteria. The chi2 test was used to compare the
frequency of each CV risk factor at baseline. Person-years methods
were used to estimate the rate of occurrence of each CV risk factor
during follow-up. Cox models were used to examine the influence
of CV risk factors on the development of CV outcomes.
RESULTS A total of 603 RA and 603 non-RA subjects (73%
female; mean age 58 years) were followed for a mean of 15 and
17 years (total: 8842 and 10,101 person-years), respectively.
At baseline, RA subjects were significantly more likely to be
former or current smokers when compared to non-RA subjects (p<0.001).
Male gender, smoking, and personal cardiac history had weaker
associations with CV events among RA subjects, compared to non-RA
subjects. There was no significant difference between RA and non-RA
subjects in the risk imparted with respect to the other CV risk
factors (ie, family cardiac history, hypertension, dyslipidaemia,
body mass index, or diabetes mellitus).
CONCLUSION While some traditional CV risk factors imparted
similar risk among RA compared with non-RA subjects, others (ie,
male gender, smoking and personal cardiac history) imparted significantly
less risk for the development of CV disease. These differences
in the overall impact of traditional CV risk factors suggest that
strategies to prevent CV disease and mortality focused solely
on controlling traditional CV risk factors may be relatively less
beneficial in RA subjects than in the general population. Further
research is needed to determine optimal approaches to reducing
CV morbidity and mortality in persons with RA.
|
| |
|
|