|
|
|
|
|
|
|
BLOCCANTI
DEI CANALI DEL CALCIO E RIFUZIONE DEL RISCHIO DI PARKINSON
[USE OF ANTIHYPERTENSIVES AND THE RISK OF PARKINSON
DISEASE. Neurology, pubblicato on line il 6 febbraio 2008]
ABSTRACT
BACKGROUND Recent studies related angiotensin converting
enzyme (ACE) inhibitors and calcium channel blockers to possible
neuroprotective effects. Little is known about neuroprotection of
angiotensin II (AT II) antagonists or beta-blockers.
OBJECTIVE To explore the association between antihypertensive
drug use and the risk of developing a first-time diagnosis of Parkinson
disease (PD).
METHODS This was a case-control analysis within the UK-based
General Practice Research Database. Cases were >/=40 years of
age with an incident PD diagnosis between 1994 and 2005. We matched
one control to each PD case on age, sex, general practice, index
date, and duration of previous history in the database. We assessed
antihypertensive drug use by timing and by exposure duration. We
calculated ORs using conditional logistic regression, adjusted for
body mass index, smoking, and various cardiovascular, metabolic,
and psychiatric diseases and dementia. RESULTS We identified 3,637
cases with a first-time diagnosis of idiopathic PD and an equal
number of matched controls. As compared to nonuse of antihypertensive
drugs, the adjusted OR for current use of >/=30 prescriptions
was 1.08 (95% CI 0.85 to 1.37) for ACE inhibitors, 0.91 (95% CI
0.41 to 2.00) for AT II antagonists, 1.16 (95% CI 0.95 to 1.41)
for beta-blockers, and 0.77 (95% CI 0.63 to 0.95) for calcium channel
blockers.
CONCLUSIONS Current long-term use of calcium channel blockers
was associated with a significantly reduced risk of a Parkinson
disease diagnosis, while the risk was not materially altered for
users of angiotensin converting enzyme inhibitors or beta-blockers
and, with less statistical precision, for users of angiotensin II
antagonists.
|
|
|
|
|
|
FARMACI
PER LE OSSA E RIDUZIONE DEL RISCHIO DI FRATTURE DA OSTEOPOROSI
[POPULATION-BASED STUDY OF THE EFFECTIVENESS OF BONE-SPECIFIC
DRUGS IN REDUCING THE RISK OF OSTEOPOROTIC FRACTUREY. Pharmacoepidemiol
Drug Saf, pubblicato on line il 23 gennaio 2008]
SUMMARY
AIM Evidence supports bone-specific drugs (BSDs) efficacy
in the fracture risk reduction. But treatment rates for osteoporosis
among high-risk patients are far below the recommended guidelines.
A major concern about BSDs is the lack of adherence with treatment.
OBJECTIVE To determine if BSDs decrease fracture risk in
high-risk elderly women in real clinical setting.
METHODS A nested case-control design was used in a cohort
of elderly women from the Quebec health databases. Women enter into
the cohort if they are 70 years or older between 1995 and 2003.
Nested case-controls were designed for women with a diagnosis of
osteoporosis (OP) and for those with a prior fracture. All cases
of fractures occurring during follow-up were matched with 10 randomly
selected controls based on age, time period, bone mass density testing,
and having a diagnosis of OP or a prior fracture. Use of BSDs before
the index date was categorized as follows: short-term (_1 year),
intermediate-term (>1 and_3 years), and long-term (>3 years).We
used an adjusted conditional logistic regression model to assess
BSD effect on fracture.
RESULTS Among 3170 women who had a fracture, of these women,
1824 had OP and 1346 had a prior fracture. Only long-term exposure
to BSDs among women with OP reduced the fracture risk by 16% (odds
ratio: 0.84; 0.73-0.97). Among women with OP, a high number of medical
services or use of anticonvulsants or narcotics increased the fracture
risk by 12-73%. Among women with a prior fracture, a high number
of medical services or risk of fall or use of benzodiazepines, antidepressants,
or narcotics increased the fracture risk by 23-77%.
CONCLUSION The incidence of fractures decreased by 16% among
women with OP when more than 80% of BSDs was used for at least 3
years. Among women with a prior fracture, fracture risk reduction
was not significant. Exposure to BSDs among women with a prior fracture
is troubling, given that only approximately 12% of these individuals
were being treated, and only 2% was using BSDs for the long term.
|
|
|
|
|
|
FATTORI
DI RISCHIO PER LE FRATTURE IN DONNE IN MENOPAUSA CON OSTEOPOROSI
[CLINICAL RISK FACTORS FOR FRACTURE IN POSTMENOPAUSAL
OSTEOPOROTIC WOMEN: A REVIEW OF THE RECENT LITERATURE. Ann Pharmacother,
pubblicato on line il 29 gennaio 2008]
ABSTRACT
OBJECTIVE To review recent literature regarding relationships
among age, weight or body mass index (BMI), bone mineral density
(BMD), maternal history of fracture, or personal prior history of
fracture and fragility fractures in women with postmenopausal osteoporosis
(PMO).
DATA SOURCES A MEDLINE database search (1995-June 30, 2007)
was conducted to identify literature related to risk factors of
interest for PMO-related fractures.
STUDY SELECTION AND DATA EXTRACTION Cohort studies, case-control
studies, and meta-analyses that reported fracture outcomes were
included if they provided an estimate of relative risk for at least
1 of the 5 selected clinical risk factors (CRFs) and studied women
with PMO or stratified risk estimates by age and sex. Of 313 identified
studies that evaluated fractures as an endpoint, 245 did not report
risk estimates for a CRF of interest and/or did not report data
for a PMO population.
DATA SYNTHESIS In the 68 included articles, the risks associated
with the evaluated CRFs were high and significant. Prior fracture
was a strong predictor of fracture and increased risk up to 18 times.
Each standard deviation below the referent mean for BMD was associated
with an increased fracture risk of up to 4.0 times; maternal fracture
history increased risk 1.3-2.9 times. Age (per 5 year increment)
increased risk by 1.2-5.0 times; low weight or BMI inconsistently
showed a 0.5-3.0 times greater risk.
CONCLUSIONS Low BMD is widely used as a diagnostic indicator
for osteoporosis; however, other CRFs play an important role in
determining fracture risk among women with PMO.
|
|
|
|
|
|
RUMORE
NOTTURNO E PRESSIONE ARTERIOSA
[ACUTE EFFECTS OF NIGHT-TIME NOISE EXPOSURE ON BLOOD
PRESSURE IN POPULATIONS LIVING NEAR AIRPORTS. Eur Heart J, pubblicato
on line il 12 febbraio 2008]
ABSTRACT
AIMS Within the framework of the HYENA (hypertension and
exposure to noise near airports) project we investigated the effect
of short-term changes of transportation or indoor noise levels on
blood pressure (BP) and heart rate (HR) during night-time sleep
in 140 subjects living near four major European airports.
METHODS AND RESULTS Non-invasive ambulatory BP measurements
at 15 min intervals were performed. Noise was measured during the
night sleeping period and recorded digitally for the identification
of the source of a noise event. Exposure variables included equivalent
noise level over 1 and 15 min and presence/absence of event (with
LAmax > 35 dB) before each BP measurement. Random effects models
for repeated measurements were applied. An increase in BP (6.2 mmHg
(0.63-12) for systolic and 7.4 mmHg (3.1, 12) for diastolic) was
observed over 15 min intervals in which an aircraft event occurred.
A non-significant increase in HR was also observed (by 5.4 b.p.m.).
Less consistent effects were observed on HR. When the actual maximum
noise level of an event was assessed there were no systematic differences
in the effects according to the noise source.
CONCLUSION Effects of noise exposure on elevated subsequent
BP measurements were clearly shown. The effect size of the noise
level appears to be independent of the noise source.
Figure 1 Box plots of the various noise indicators measured during
the study night
[HYPERTENSION AND EXPOSURE TO NOISE NEAR AIRPORTS: THE HYENA
STUDY. Environ Health Perspect 2008; 116:329-333]
ABSTRACT
BACKGROUND An increasing number of people are exposed to
aircraft and road traffic noise. Hypertension is an important risk
factor for cardiovascular disease, and even a small contribution
in risk from environmental factors may have a major impact on public
health.
OBJECTIVES The HYENA (Hypertension and Exposure to
Noise near Airports) study aimed to assess the relations between
noise from aircraft or road traffic near airports and the risk of
hypertension.
METHODS We measured blood pressure and collected data on
health, socioeconomic, and lifestyle factors, including diet and
physical activity, via questionnaire at home visits for 4,861 persons
45-70 years of age, who had lived at least 5 years near any of six
major European airports. We assessed noise exposure using detailed
models with a resolution of 1 dB (5 dB for United Kingdom road traffic
noise) , and a spatial resolution of 250 250 m for aircraft and
10 10 m for road traffic noise.
RESULTS We found significant exposure-response relationships
between night-time aircraft as well as average daily road traffic
noise exposure and risk of hypertension after adjustment for major
confounders. For night-time aircraft noise, a 10-dB increase in
exposure was associated with an odds ratio (OR) of 1.14 [95% confidence
interval (CI) , 1.01-1.29]. The exposure-response relationships
were similar for road traffic noise and stronger for men with an
OR of 1.54 (95% CI, 0.99-2.40) in the highest exposure category
(> 65 dB ; ptrend = 0.008) .
CONCLUSIONS Our results indicate excess risks of hypertension
related to long-term noise exposure, primarily for night-time aircraft
noise and daily average road traffic noise.
|
|
|
|
|
|
BIOMARKER
PROTEOMICI URINARI E CORONAROPATIA
[URINARY PROTEOMIC BIOMARKERS IN CORONARY ARTERY
DISEASE. Mol Cell Proteomics 2008; 7:290-298]
ABSTRACT
Urinary proteomics is emerging as a powerful non-invasive tool for
diagnosis and monitoring of variety of human diseases. We tested
whether signatures of urinary polypeptides can contribute to the
existing biomarkers for coronary artery disease (CAD). We examined
a total of 359 urine samples from 88 patients with severe CAD and
282 controls. Spot urine was analyzed using capillary electrophoresis
on-line coupled to ESI-TOF-MS enabling characterization of more
than 1000 polypeptides per sample. In a first step a "training
set" for biomarker definition was created. Multiple biomarker
patterns clearly distinguished healthy controls from CAD patients,
and we extracted 15 peptides that define a characteristic CAD signature
panel. In a second step, the ability of the CAD-specific panel to
predict the presence of CAD was evaluated in a blinded study using
a "test set." The signature panel showed sensitivity of
98% (95% confidence interval, 88.7-99.6) and 83% specificity (95%
confidence interval, 51.6-97.4). Furthermore the peptide pattern
significantly changed toward the healthy signature correlating with
the level of physical activity after therapeutic intervention. Our
results show that urinary proteomics can identify CAD patients with
high confidence and might also play a role in monitoring the effects
of therapeutic interventions. The workflow is amenable to clinical
routine testing suggesting that non-invasive proteomics analysis
can become a valuable addition to other biomarkers used in cardiovascular
risk assessment.
|
|
|
|
|
|
LP-PLA2
E CORONAROPATIA
[LIPOPROTEIN-ASSOCIATED PHOSPHOLIPASE A2 IS AN INDEPENDENT
PREDICTOR OF INCIDENT CORONARY HEART DISEASE IN AN APPARENTLY HEALTHY
OLDER POPULATION: THE RANCHO BERNARDO STUDY. J Am Coll Cardiol 2008;
51:913-919]
ABSTRACT
OBJECTIVES Lipoprotein-associated phospholipase A2 (Lp-PLA2)
levels predict incident coronary heart disease (CHD) in adults without
known CHD, independent of heart disease risk factors. We examined
whether the independent association was apparent in older adults.
BACKGROUND Serum levels of Lp-PLA2, an enzyme that hydrolyzes
oxidized phospholipids to yield potentially proatherogenic particles,
have been associated with CHD and may help predict cardiovascular
risk.
METHODS Participants were 1,077 community-dwelling men and
women, median age 72 years, who had no known CHD at baseline (1984
to 1987) when blood samples and risk factor data were collected.
Participants were followed for CHD events for a mean of 16 years,
through 2002. Cox proportional hazards regression models were used
to examine the association of serum Lp-PLA2 with incident CHD (myocardial
infarction, angina, or coronary revascularization).
RESULTS The Lp-PLA2 levels positively correlated with age
(r = 0.09), body mass index (r = 0.11), low-density lipoprotein
(r = 0.37), triglycerides (r = 0.25), and C-reactive protein (r
= 0.10), and negatively correlated with high-density lipoprotein
(r = -0.27) (all p < 0.05). During follow-up, 228 participants
had incident CHD events. Lipoprotein-associated phospholipase A2
levels in the second, third, and fourth quartiles predicted an increased
risk of CHD compared with the lowest quartile (hazard ratios 1.66,
1.80, and 1.89, respectively; p < 0.05 for each). This association
persisted after adjusting for C-reactive protein and other CHD risk
factors.
CONCLUSIONS Elevated Lp-PLA2 levels predict CHD events in
apparently healthy older adults, independent of CHD risk factors.
|
|
|
|
|
|
SINDROME
METABOLICA E FIBRILLAZIONE ATRIALE
[METABOLIC SYNDROME AND RISK OF DEVELOPMENT OF ATRIAL
FIBRILLATION. THE NIIGATA PREVENTIVE MEDICINE STUDY. Circulation,
pubblicato on line il 19 febbraio 2008]
ABSTRACT
BACKGROUND The metabolic syndrome consists of a cluster of
atherosclerotic risk factors, many of which also have been implicated
in the genesis of atrial fibrillation (AF). However, the precise
role of the metabolic syndrome in the development of AF is unknown.
METHODS AND RESULTS This prospective, community-based, observational
cohort study was based on an annual health check-up program in Japan.
We studied 28 449 participants without baseline AF. We used 2 different
criteria for the metabolic syndrome-the guidelines of the National
Cholesterol Education Program Third Adult Treatment Panel (NCEP-ATP
III) and those of the American Heart Association/National Heart,
Lung, and Blood Institute (AHA/NHLBI)-to study the risk of development
of new-onset AF. The metabolic syndrome was present in 3716 subjects
(13%) and 4544 subjects (16%) using the NCEP-ATP III and AHA/NHLBI
definitions, respectively. During a mean follow-up of 4.5 years,
AF developed in 265 subjects (105 women). Among the metabolic syndrome
components, obesity (age- and sex-adjusted hazard ratio [HR], 1.64),
elevated blood pressure (HR, 1.69), low high-density lipoprotein
cholesterol (HR, 1.52), and impaired insulin tolerance (HR, 1.44
[NCEP-ATP III] and 1.35 [AHA/NHLBI]) showed an increased risk for
AF. The association between the metabolic syndrome and AF remained
significant in subjects without treated hypertension or diabetes
by the NCEP-ATP III definition (HR, 1.78) but not by the AHA/NHLBI
definition (HR, 1.28).
CONCLUSIONS The metabolic syndrome was associated with increased
risk of AF. The metabolic derangements of the syndrome may be important
in the pathogenesis of AF.
|
|
|
|
|
|
STRESS
LAVORATIVO E MALATTIE CORONARICHE
[WORK STRESS AND CORONARY HEART DISEASE: WHAT ARE
THE MECHANISMS? Eur Heart J, pubblicato on line il 23 gennaio 2008]
ABSTRACT
AIMS To determine the biological and behavioural factors
linking work stress with coronary heart disease (CHD).
METHODS AND RESULTS A total of 10 308 London-based male and
female civil servants aged 35-55 at phase 1 (1985-88) of the Whitehall
II study were studied. Exposures included work stress (assessed
at phases 1 and 2), and outcomes included behavioural risk factors
(phase 3), the metabolic syndrome (phase 3), heart rate variability,
morning rise in cortisol (phase 7), and incident CHD (phases 2-7)
on the basis of CHD death, non-fatal myocardial infarction, or definite
angina. Chronic work stress was associated with CHD and this association
was stronger among participants aged under 50 (RR 1.68, 95% CI 1.17-2.42).
There were similar associations between work stress and low physical
activity, poor diet, the metabolic syndrome, its components, and
lower heart rate variability. Cross-sectionally, work stress was
associated with a higher morning rise in cortisol. Around 32% of
the effect of work stress on CHD was attributable to its effect
on health behaviours and the metabolic syndrome.
CONCLUSION Work stress may be an important determinant of
CHD among working-age populations, which is mediated through indirect
effects on health behaviours and direct effects on neuroendocrine
stress pathways.
|
|
|
|
|
|
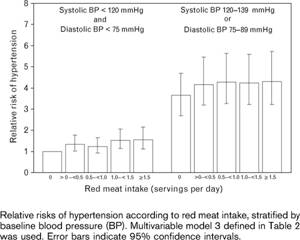
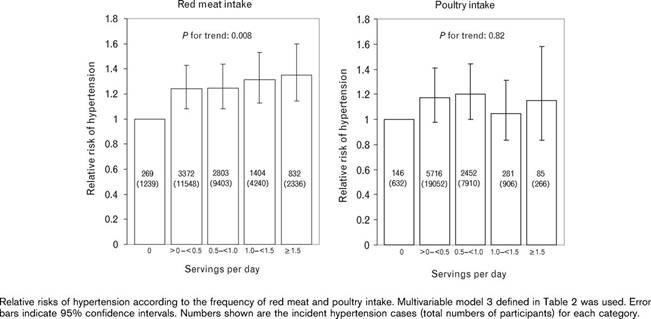
CONSUMO
DI CARNE E RISCHIO DI IPERTENSIONE IN DONNE DI MEZZA ETÀ
E ANZIANE
[MEAT INTAKE AND THE RISK OF HYPERTENSION IN MIDDLE-AGED
AND OLDER WOMEN. J Hyper 2008; 26:215-222]
ABSTRACT
BACKGROUND Although previous studies have suggested that
high intake of meat, particularly red meat, may contribute to
the development of hypertension, data on the prospective associations
between meat intake and risk of hypertension are still limited.
OBJECTIVE We investigated the association of total red
meat, types of red meat and poultry intake at baseline with the
incidence of hypertension in a prospective cohort of 28 766 female
US health professionals aged >= 45 years.
PATIENTS AND METHODS Baseline red meat and poultry intake
were assessed from semiquantitative food frequency questionnaires.
Incident cases of hypertension (n = 8693) were identified from
annual follow-up questionnaires during 10 years of follow-up.
RESULTS After adjusting for known hypertension risk factors,
the relative risk and 95% confidence interval (CI) of incident
hypertension were 1.00 (reference), 1.05 (0.97-1.13), 1.05 (0.97-1.13),
1.05 (0.97-1.14) and 1.13 (1.04-1.23), respectively, across increasing
quintiles of baseline total red meat intake (P for trend = 0.008).
Using functional cutpoints, women who consumed > 0 to <
0.5, 0.5 to < 1.0, 1.0 to < 1.5 and >= 1.5 servings/day
of total red meat had multivariable relative risks (95% CI) of
hypertension of 1.24 (1.08-1.43), 1.25 (1.08-1.44), 1.32 (1.13-1.53)
and 1.35 (1.14-1.59) compared to those who consumed no red meat
(P for trend = 0.008). By contrast, multivariable relative risks
of incident hypertension across increasing quintiles of poultry
intake were 1.00, 1.03, 1.03, 1.08 and 1.03 (P for trend = 0.37).
CONCLUSIONS Red meat intake was positively associated,
whereas poultry intake was unassociated, with the risk of hypertension
in middle-aged and older women.
|
|
|
|
|
|
CONSUMO
DI ALCOLICI NEL CORSO DELLA VITA E RISCHIO CARDIOMETABOLICO
[ASSOCIATION OF LIFETIME ALCOHOL DRINKING TRAJECTORIES
WITH CARDIOMETABOLIC RISK. J Clin Endocrinol Metab 2008; 93:154-61]
ABSTRACT
CONTEXT AND OBJECTIVE Alcohol intakes may vary considerably
over a drinker's lifetime. This study was designed to examine whether
lifetime drinking trajectories are associated with cardiovascular
risk factors that are used to define the metabolic syndrome (MetS).
DESIGN, SETTING, PARTICIPANTS AND OUTCOMES This is a population-based
cross-sectional study. Participants were ever-regular drinkers (n
= 2818) selected from healthy controls for the Western New York
Health Study (1996-2001) in which lifetime lifestyle was ascertained
retrospectively. Prevalence of the MetS and its individual components,
including obesity, high triglycerides, low high-density lipoprotein
cholesterol, elevated blood pressure, and high fasting glucose,
were the main outcomes.
RESULTS Trajectory analyses were based on estimates of total
kilograms of ethanol for each age decade between 10 and 59 yr. Two
groups of drinkers with distinct lifetime drinking trajectories
were obtained, an early peak and a stable trajectory group. Compared
with stable trajectory drinkers, early-peak drinkers were 10 yr
younger on average, had earlier onset of regular drinking, drank
heavily in late adolescence and early adulthood tapering off in
middle age, averaged more drinks per drinking day in lifetime, and
were more likely to abstain when interviewed. After controlling
for age, sex, and other potential confounders, early-peak trajectories
were modestly associated with high odds of the MetS [1.31; 95% confidence
interval (CI) 1.00, 1.71] overall, low high-density lipoprotein
cholesterol (1.62; 95% CI 1.27, 2.08), abdominal obesity (1.48;
95% CI 1.23, 1.78), and overweight (1.32; 95% CI 1.10, 1.60).
CONCLUSION Early initiation of alcohol drinking and heavy
drinking in adolescence and early adulthood may be associated with
an adverse cardiometabolic profile.
|
|
|
|
|
|
SOFT
DRINKS E RISCHIO DI GOTTA NEGLI UOMINI
[SOFT DRINKS, FRUCTOSE CONSUMPTION, AND THE RISK
OF GOUT IN MEN: PROSPECTIVE COHORT STUDY. BMJ 2008; 336:309-12]
ABSTRACT
OBJECTIVE To examine the relation between intake of sugar
sweetened soft drinks and fructose and the risk of incident gout
in men.
DESIGN Prospective cohort over 12 years.
SETTING Health professionals follow-up study.
PARTICIPANTS 46 393 men with no history of gout at baseline
who provided information on intake of soft drinks and fructose through
validated food frequency questionnaires.
MAIN OUTCOME MEASURE Incident cases of gout meeting the American
College of Rheumatology survey criteria for gout.
RESULTS During the 12 years of follow-up 755 confirmed incident
cases of gout were reported. Increasing intake of sugar sweetened
soft drinks was associated with an increasing risk of gout. Compared
with consumption of less than one serving of sugar sweetened soft
drinks a month the multivariate relative risk of gout for 5-6 servings
a week was 1.29 (95% confidence interval 1.00 to 1.68), for one
serving a day was 1.45 (1.02 to 2.08), and for two or more servings
a day was 1.85 (1.08 to 3.16; P for trend=0.002). Diet soft drinks
were not associated with risk of gout (P for trend=0.99). The multivariate
relative risk of gout according to increasing fifths of fructose
intake were 1.00, 1.29, 1.41, 1.84, and 2.02 (1.49 to 2.75; P for
trend <0.001). Other major contributors to fructose intake such
as total fruit juice or fructose rich fruits (apples and oranges)
were also associated with a higher risk of gout (P values for trend
<0.05).
CONCLUSIONS Prospective data suggest that consumption of
sugar sweetened soft drinks and fructose is strongly associated
with an increased risk of gout in men. Furthermore, fructose rich
fruits and fruit juices may also increase the risk. Diet soft drinks
were not associated with the risk of gout.
FIG 1: Rischio relativo multivariato per quintili di apporto di
fruttosio. Il gruppo di riferimento è il quintile inferiore
e con IMC<25 kg/m2 (in alto), nessun uso di alcol (in mezzo)
e 1,6 porzioni di latticini giornaliere (in basso). Il rischio relativo
è aggiustato per età, apporto energetico totale, indice
di massa corporea, uso di diuretici, storia di ipertensione, storia
di insufficienza renale, consumo di alcol, apporto totale di vitamina
C e percentuale di energia sul totale di carboidrati e proteine.
|
|
|
|
|
|
APPORTO
DIETETICO DI VITAMINA B3 E CANCRO COLORETTALE
[DIETARY VITAMIN B6 INTAKE AND THE RISK OF COLORECTAL
CANCER. Cancer Epidemiol Biomarkers Prev 2008; 17:171-182]
ABSTRACT
Vitamin B6, a coenzyme in the folate metabolism pathway, may have
anticarcinogenic effects. Laboratory and epidemiologic studies support
the hypothesis of its protective effect against colorectal cancer
(CRC). The aim of this large Scottish case-control study, including
2,028 hospital-based cases and 2,722 population-based controls,
was to investigate the associations between dietary and supplementary
intake of vitamin B6 and CRC. Three logistic regression models adjusted
for several confounding factors, including energy, folate, and fiber
intake, were applied in the whole sample and after age, sex, cancer
site, folate, MTHFR C677T (rs1801133), MTHFR A1298C (rs1801131),
MTR A2756G (rs1805087), and MTRR A66G (rs1801394) stratification
(analysis on genotypes on 1,001 cases and 1,010 controls </=55
years old). Moderately strong inverse and dose-dependent associations
in the whole sample were found between CRC risk and the intake of
dietary and total vitamin B6 in all three models [model III: odds
ratio (OR), 0.77; 95% confidence interval (95% CI), 0.61-0.98; P
for trend = 0.03; OR, 0.86; 95% CI, 0.69-1.07; P for trend = 0.12].
In addition, meta-analyses of published studies showed inverse associations
between vitamin B6 and CRC (combined relative risk, 0.81; 95% CI,
0.68-0.96; test for overall effect P = 0.01; combined odds ratio,
0.67; 95% CI, 0.60-0.75; test for overall effect P < 0.00001).
Analysis within the stratified subgroups showed similar associations
apart from a stronger effect among </=55-year-old individuals.
Evidence from larger cohort and experimental studies is now required
to confirm and define the anticarcinogenic actions of vitamin B6
and to explore the mechanisms by which this effect is mediated.
|
|
|
|
|
|
INDICE
DI MASSA CORPOREA E INCIDENZA DI CANCRO
[BODY-MASS INDEX AND INCIDENCE OF CANCER: A SYSTEMATIC
REVIEW AND META-ANALYSIS OF PROSPECTIVE OBSERVATIONAL STUDIES.
The Lancet 2008; 371:569-578]
SUMMARY
BACKGROUND Excess bodyweight, expressed as increased body-mass
index (BMI), is associated with the risk of some common adult
cancers. We did a systematic review and meta-analysis to assess
the strength of associations between BMI and different sites of
cancer and to investigate differences in these associations between
sex and ethnic groups.
METHODS We did electronic searches on Medline and Embase
(1966 to November 2007), and searched reports to identify prospective
studies of incident cases of 20 cancer types. We did random-effects
meta-analyses and meta-regressions of study-specific incremental
estimates to determine the risk of cancer associated with a 5
kg/m2 increase in BMI.
FINDINGS We analysed 221 datasets (141 articles), including
282?137 incident cases. In men, a 5 kg/m2 increase in BMI was
strongly associated with oesophageal adenocarcinoma (RR 1·52,
p<0·0001) and with thyroid (1·33, p=0·02),
colon (1·24, p<0·0001), and renal (1·24,
p <0·0001) cancers. In women, we recorded strong associations
between a 5 kg/m2 increase in BMI and endometrial (1·59,
p<0·0001), gallbladder (1·59, p=0.04), oesophageal
adenocarcinoma (1·51, p<0·0001), and renal (1·34,
p<0·0001) cancers. We noted weaker positive associations
(RR <1·20) between increased BMI and rectal cancer and
malignant melanoma in men; postmenopausal breast, pancreatic,
thyroid, and colon cancers in women; and leukaemia, multiple myeloma,
and non-Hodgkin lymphoma in both sexes. Associations were stronger
in men than in women for colon (p<0·0001) cancer. Associations
were generally similar in studies from North America, Europe and
Australia, and the Asia-Pacific region, but we recorded stronger
associations in Asia-Pacific populations between increased BMI
and premenopausal (p=0·009) and postmenopausal (p=0·06)
breast cancers.
INTERPRETATION Increased BMI is associated with increased
risk of common and less common malignancies. For some cancer types,
associations differ between sexes and populations of different
ethnic origins. These epidemiological observations should inform
the exploration of biological mechanisms that link obesity with
cancer.
|
|
|
|
| |
FATTORI
DI RISCHIO PER LA PSORIASI
[MEDICAL HISTORY, DRUG EXPOSURE AND THE RISK OF PSORIASIS.
EVIDENCE FROM AN ITALIAN CASE-CONTROL STUDY. Dermatology 2008; 216:125-30]
ABSTRACT
BACKGROUND/AIMS To evaluate the association of psoriasis
with selected medical conditions and a number of drugs used before
diagnosis.
METHODS Multicenter case-control study involving outpatient
services of 20 general and teaching hospitals. Entry criteria for
cases were a first diagnosis of psoriasis made by a dermatologist
and a history of skin manifestations of no more than 2 years after
the reported onset of the disease. Controls were the first eligible
dermatological patients observed on randomly selected days in the
same centers as cases. A total of 560 cases and 690 controls were
recruited.
RESULTS The odds ratio (OR) of psoriasis was 0.8 (95% confidence
interval, CI, 0.5-1.3) in hypertensive subjects, 1.1 (95% CI 0.6-2.0)
in diabetics and 1.1 (95% CI 0.7-1.7) in hyperlipidemic subjects.
Histamine 2 receptor antagonist exposure was negatively associated
with psoriasis: OR 0.3 (95% CI 0.1-0.8).
CONCLUSION Our study rules out a strong association of psoriasis
at its first ever diagnosis with common chronic conditions. The
reported associations of psoriasis with relatively common conditions
such as diabetes mellitus, hypertension and hyperlipidemia may represent
a late effect of well-known risk factors for psoriasis such as smoking
and overweight or reflect factors related to the long course of
psoriasis itself.
[ASSOCIATION BETWEEN PSORIASIS AND THE METABOLIC SYNDROME. A
CROSS-SECTIONAL STUDY. Dermatology 2008; 216:152-5]
ABSTRACT
BACKGROUND Previous reports have shown an association between
inflammatory diseases such as systemic lupus erythematosus or rheumatoid
arthritis and the metabolic syndrome. Recent data demonstrate that
psoriasis is an inflammatory disease, suggesting that psoriasis
may be one of the components of the metabolic syndrome.
OBJECTIVE To assess the association between psoriasis and
the metabolic syndrome.
METHODS A cross-sectional study was performed utilizing the
database of the Clalit Health Services. Case patients were defined
as patients with a diagnosis of psoriasis vulgaris. Controls were
randomly selected from the list of Clalit Health Services enrollees.
The proportions of components of the metabolic syndrome (ischemic
heart disease, hypertension, diabetes, obesity and dyslipidemia)
were compared between case and control patients by univariate analyses.
chi(2) tests were used to compare categorical parameters between
the groups. Logistic and linear regression models served to measure
the association between psoriasis and the metabolic syndrome.
RESULTS The study included 16,851 patients with psoriasis
and 48,681 controls. In the case group, there were 8,449 men (50.1%)
and 8,402 women (49.9%), with a mean age of 42.7 years (SD = 20.3,
range = 2-111). Diabetes mellitus was present in 13.8% of the patients
with psoriasis as compared to 7.3% of the controls (p < 0.001).
Hypertension occurred in 27.5% of the patients with psoriasis and
in 14.4% of the controls (p < 0.001). Obesity was present in
8.4% of the patients with psoriasis as opposed to 3.6% of the controls
(p < 0.001). Ischemic heart disease was observed in 14.2% of
the patients with psoriasis as compared to 7.1% of the controls
(p < 0.001). Multivariate models adjusting for age, gender and
smoking status of the patients demonstrated that psoriasis was associated
with the metabolic syndrome (OR = 1.3, 95% CI = 1.1-1.4), ischemic
heart disease (OR = 1.1, 95% CI = 1.0-1.2), diabetes mellitus (OR
= 1.2, 95% CI = 1.0-1.3), hypertension (OR = 1.3, 95% CI = 1.2-1.5)
and obesity (OR = 1.7, 95% CI = 1.5-1.9).
LIMITATIONS The study is designed as a case-control study,
thus an association alone was proven and not causality.
CONCLUSION Our findings demonstrate a possible association
between psoriasis and the metabolic syndrome. Appropriate treatment
of the metabolic syndrome may be an important part of the management
of patients with psoriasis.
|
|
|
|
| |
SVILUPPO
E VALIDAZIONE DI UN RISK SCORE PER L'OSTEOPOROSI NEGLI UOMINI
[DEVELOPMENT AND INTERNAL VALIDATION OF THE MALE
OSTEOPOROSIS RISK ESTIMATION SCORE. Ann Fam Med 2007; 5:540-6]
ABSTRACT
PURPOSE We wanted to develop and validate a clinical prediction
rule to identify men at risk for osteoporosis and subsequent hip
fracture who might benefit from dual-energy x-ray absorptiometry
(DXA).
METHODS We used risk factor data from the National Health
and Nutrition Examination Survey III to develop a best fitting
multivariable logistic regression model in men aged 50 years and
older randomized to either the development (n = 1,497) or validation
(n = 1,498) cohorts. The best fitting model was transformed into
a simplified scoring algorithm, the Male Osteoporosis Risk Estimation
Score (MORES). We validated the MORES, comparing sensitivity,
specificity, and area under the receiver operating characteristics
(ROC) curve in the 2 cohorts and assessed clinical utility with
an analysis of the number needed-to-screen (NNS) to prevent 1
additional hip fracture.
RESULTS The MORES included 3 variables-age, weight, and
history of chronic obstructive pulmonary disease-and showed excellent
predictive validity in the validation cohort. A score of 6 or
greater yielded an overall sensitivity of 0.93 (95% CI, 0.85-0.97),
a specificity of 0.59 (95% CI, 0.56-0.62), and an area under the
ROC curve of 0.832 (95% CI, 0.807-0.858). The overall NNS to prevent
1 additional hip fracture was 279 in a cohort of men representative
of the US population.
CONCLUSIONS Osteoporosis is a major predictor of hip fractures.
Experts believe bisphosphonate treatment in men should yield results
similar to that in women and reduce hip fracture rates associated
with osteoporosis. In men aged 60 years and older, the MORES is
a simple approach to identify men at risk for osteoporosis and
refer them for confirmatory DXA scans.
MALE
OSTEOPOROSIS RISK ESTIMATION SCORE (MORES)
| RISK
FACTOR |
LOGISTIC
REGRESSION beta-COEFFICIENT |
MORES
POINTS (*) |
| Age |
55
years (§) |
0.00
|
0
|
| 56-74
years |
1.29
|
3
|
| 75
years |
2.03
|
4
|
| Weight |
70
kg ( 154 lb) |
3.07
|
6
|
| >70-80
kg (>154-176 lb) |
1.86
|
4
|
| >80
kg (>176 lb) (§) |
0.00
|
0
|
| COPD |
1.32
|
3
|
COPD
= chronic obstructive pulmonary disease.
* Screening threshold is 6 points or greater.
§ Reference category.
|
|
|
|
| |
|
|